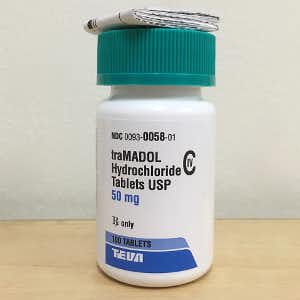
Almost everyone has heard about the opioid epidemic. According to the National Institute on Drug Abuse, “Every day, more than 130 people in the United States die after overdosing on opioids.” What has not made headlines, however, are the potential problems with alternate pain medicines. Many doctors are now prescribing tramadol, a key ingredient in the brand name pain reliever, Ultracet. This reader says that stopping Ultracet was challenging.
How Should You Stop Ultracet?
Q. I started taking Ultracet about a year ago. This medicine contains tramadol and acetaminophen.
I began with just one a day. In less than a month, I was taking five pills a day. Now I want to get off this medication. Should I start by tapering the dosage? Or just stop it altogether?
Three days have passed since I took my last tablet. I haven’t slept during that time and I’m feeling anxious and sweaty. If these symptoms don’t increase, I will be able to continue without medication. But if they get worse, I wouldn’t know what to do!
A. When tramadol was first introduced, the maker presented it as an alternative to narcotic pain relievers. It has since become clear that some people can become dependent on tramadol. Stopping Ultracet suddenly can be challenging. Sadly, neither the FDA nor the manufacturer give clear guidelines about how to taper off Ultracet or tramadol.
What’s the Story on Tramadol?
This drug has some opioid activity, but it also affects neurotransmitters such as serotonin and norepineprine. That means it can trigger a “discontinuation syndrome” similar to one people might experience if they abruptly stopped drugs like sertraline (Zoloft) or venlafaxine (Effexor).
Discontinuing tramadol suddenly can lead to withdrawal symptoms such as anxiety, insomnia, sweating, nausea, pain, tremors or diarrhea. A few people report panic attacks or “brain zaps.”
The Double Whammy:
Because tramadol has both weak opioid action as well as antidepressant-like neurochemistry, there could be a dual effect. Stopping Ultracet suddenly could lead to side effects such as those our reader reported.
You can learn more about tramadol side effects and withdrawal at this link.
Stories from Other Readers:
This person has had a tough time:
“My doctor first prescribed Ultram/Ultracet for my fibromyalgia about 25 years ago, when I was in my late 40s.. I took 20 mg 2 x a day so I could continue to work. The feeling when I was late with a dose was awful.
“After a few years I weaned off it very slowly and went back to work part time. Then as I got older, and arthritis and old injuries began to slow me down with more pain, I went back on it (50 mg 2 x a day). After two years and trouble sleeping the doctor increased the dose to 3 x a day.
“Now I am retired and downsized. I have been weaning myself off SLOWLY for about 5 weeks by cutting pills. I am now down to about 1/3 of the 50mg pill 3 x a day and I’m paying close attention to how I feel. Only my husband believes how bad stopping Ultracet has been. All symptoms are true, and unbelievably bad.
“In a few weeks, I will be seeing a new doctor. Hopefully, I will be done with this by then. I am eating only organic food and getting on a good schedule. I hope pain management will not be the monster it has been.
“My knees are shot, I have had spinal surgery, two shoulder surgeries, a broken ankle, etc. I am 71, I hope to get to a good place for the rest of my life.
“This all got started because my doctor told me to “take more to feel good.” I got almost no encouragement to wean off. My doctor told me,’good luck; you are brave.’ That may have been only because I had been his patient for 25 years, and I was a medical professional too.”
Tresa shared this story:
“I was on medication for depression for 2 years. Last year I fought through the withdrawal symptoms and stopped the medications completely. Recently I had a miscarriage and last week I had a hip surgery. Mostly I was on tramadol injections and when I came home they gave me 2 painkillers. One of them was Ultracet.
“I stopped it whenever I felt my pain was bearable. After a day, I had severe panic attacks. I had suicidal thoughts and sleepless nights. I was scared to death that my husband would leave me (for no reason). As a result, I cried all night.
“I was confused about what was causing all this. It is just by chance I went through the comments on the PeoplesPharmacy.com website and now I know these are withdrawal symptoms. It will be difficult at first, but I will have to do taper off this drug properly. Otherwise I will end up in that hopeless place again.
“I will be stopping Ultracet little by little. It’s difficult, but it’s possible.”
C.S. is scared and confused after stopping Ultracet:
“I’m on day 28 of Ultracet withdrawal. I was doing better after 2 weeks of hell. Cold turkey. No other choice. Now it’s like withdrawals are starting all over again. No sleep. Heart palpitations, nausea, anxiety and twitchiness 24/7 the past three days. What the hell is going on?”
Doctors are advised to reduce the dose gradually to avoid such problems. But what does “gradually” mean? Is it a week, a month, six months or longer? Without guidance many patients feel like C.S. We suspect that many people can be successful with a six-week taper, but some may need to reduce the dose even more gradually.
Share your own experience with Ultracet or tramadol in the comment section below.

