Stopping Airborne Viruses
Do you worry about things you can’t see, smell or taste? Most of us don’t. Yet particles we can’t detect with our five senses are often present in the air we breathe. They have the power to make us sick. How can we achieve cleaner indoor air so that we have less chance of coming down with a serious infection?
At The People’s Pharmacy, we strive to bring you up‑to‑date, rigorously researched insights and conversations about health, medicine, wellness and health policies and health systems. While these conversations intend to offer insight and perspective, the content is provided solely for informational and educational purposes. Please consult your healthcare provider before making any changes to your medical care or treatment.
How You Can Listen:
You could listen through your local public radio station or get the live stream at 7 am EST on Saturday, Dec. 6, 2025, through your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast later. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on Dec. 8, 2025.
The Importance of Cleaner Indoor Air:
When we talk about air pollution, the image that may arise is factories belching dark plumes of smoke. While the particles generated by industrial processes can be dangerous for our health, sometimes the greatest danger is from particles we can’t see.
The COVID-19 pandemic brought this into sharp focus, as we realized that people who had not yet begun to experience symptoms could be spreading infectious viruses. But the need for cleaner indoor air is not limited to COVID, or even to an epidemic like measles or the flu. Many infections spread primarily on viral particles wafting through the air. We are reminded of this every winter, as cases of influenza start to rise. But respiratory syncytial virus, human metapneumovirus and dozens of rhinoviruses and coronaviruses that cause colds also travel on the air. So do measles viruses.
Our guest, Dr. Linsey Marr, is one of the country’s leading environmental engineers. She got interested in airborne transmission of infection even before SARS-CoV-2 appeared. Then, with COVID, it became clear that the advice to the public about maintaining 6 feet of distance was inadequate to protect people from coming down with the infection. It was developed based on an outdated understanding of how infectious particles travel.
Can You Tell If Indoor Air Is Contaminated?
Given the extremely small size of viral particles, we might have to use our imagination to understand how they could be present. We can’t smell viruses. But if you imagine someone smoking a cigar in the room, you know that the smell will linger for quite a while after the smoker has left. Viral particles can float around like the smell of cigar smoke, which is why they can still be present even after an infected person has left the space.
This viral behavior means that the riskiest places are those where many people congregate, especially during a season when infections are spreading. Think of grocery stores, hospitals, or athletic event venues. Wearing a tightly fitted N95 or KN95 mask could provide some protection (especially if others also wore masks). It is not a magic bullet, though. Japanese people accept mask protocol during flu season, and they have still experienced the spread of influenza. In the US, it is very unlikely that most people will accept wearing masks, even if it could help reduce their risk of infection.
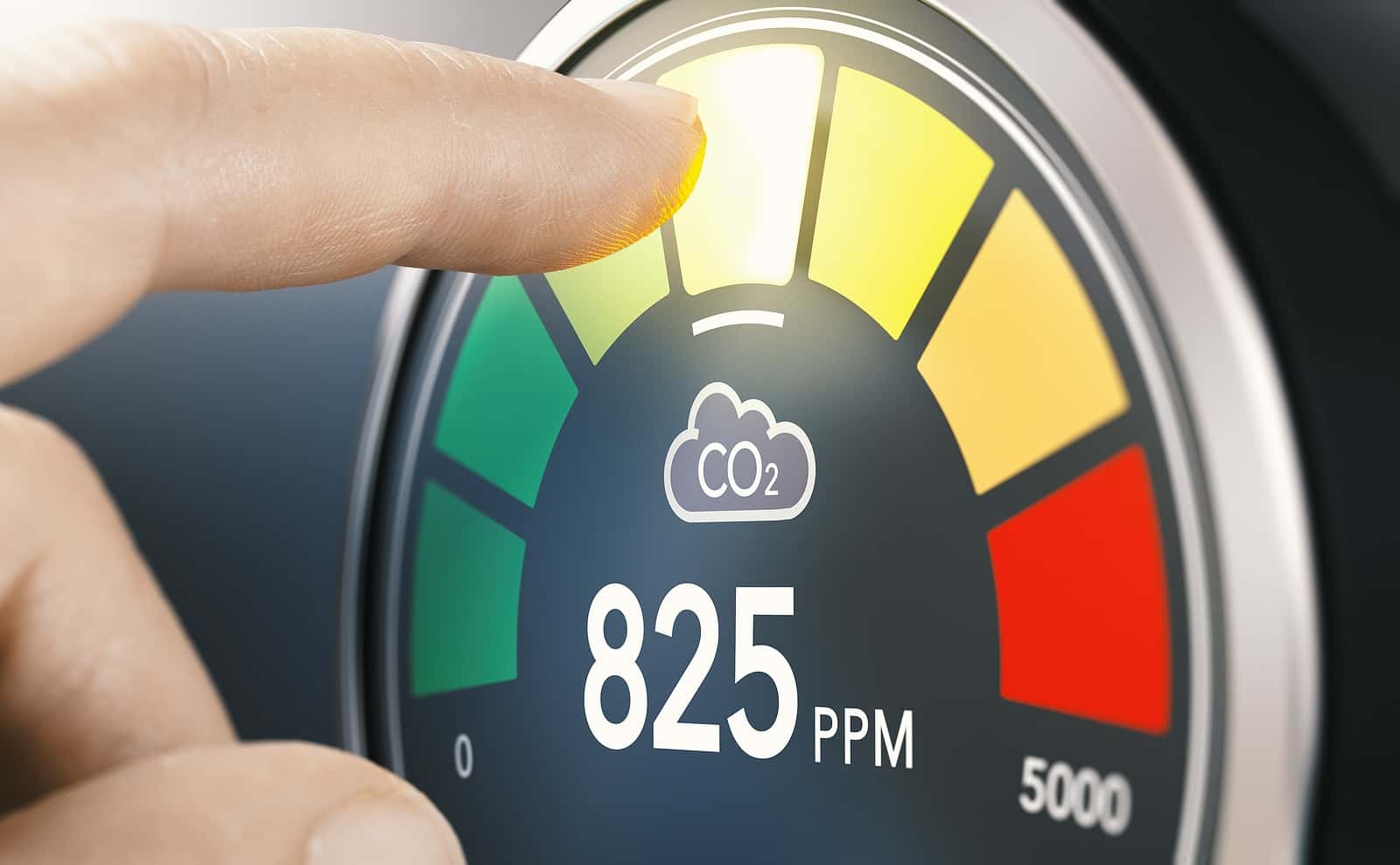
While we can’t measure viral particles in the air without complicated equipment, we can use a simple relatively inexpensive piece of equipment to check the ventilation in a space with multiple people. It is called a carbon dioxide (CO2) monitor. Because people exhale CO2, high levels of this harmless gas indicate lots of people breathing in the space without much ventilation. Fresh outdoor air runs about 400 ppm CO2. Once indoor air reaches 1,000 ppm or higher, you may want to take action.
Moving Toward Cleaner Indoor Air:
Ventilation:
Improving ventilation would be very advantageous. Most public places should strive to achieve at least 4 to 6 air exchanges per hour. More sensitive spaces such as health care facilities might benefit from a higher level of ventilation.
Filtration:
The other way to deal with airborne viruses is through filtration. Home air handling systems could be equipped with a high-efficiency particulate arresting (HEPA) filter. This is ideal, but it may not be practical in every space. Ordinary air filters carry a MERV number such as 8, 11 or 13. Higher numbers indicated better filtration capacity. In general, you’d want to use the highest MERV number your HVAC system will tolerate. Too high a number can create too much pressure and cause problems.
What if you don’t have access to the filters for your air? That is the case for many apartment dwellers who have to share their air with everyone else in the building. One affordable option is to build and use a Corsi-Rosenthal box. It can be assembled at home for $50 to $70 and it works quite well to provide cleaner indoor air in the space where it is operating. Dr. Marr describes how to build one. Here is a link to our interview with Dr. Corsi, including instructions on building a Corsi-Rosenthal box.
Elimination:
Another step toward cleaner indoor air might be to utilize ultraviolet (UV) light as a disinfectant. A unit that uses germicidal UV at a wavelength of 250 nanometers needs to be tucked into air ducts. That wavelength can damage eyes and skin. New technology is being developed using a slightly different wavelength of 222 nanometers. While still germicidal, it is supposed to be safe for human eyes.
This Week’s Guest:
Linsey Marr, PhD, is a professor of civil and environmental engineering at Virginia Tech, where she leads the Applied Interdisciplinary Research in Air (AIR2) laboratory. Her research group focuses on the dynamics of biological aerosols like viruses, bacteria, and fungi in indoor and outdoor air. Marr teaches courses in environmental engineering and air quality, including topics in the context of global climate change, as well as health and ecosystem effects. She has been thinking and writing about how to avoid airborne viral transmission since the pandemic began, as in this article published in Environment International (Sep. 2020). Photo by Peter Means, courtesy of Virginia Tech.

Dr. Linsey Marr of Virginia Tech. Photo by Peter Means, courtesy of Virginia Tech
Dr. Marr mentioned her publication, with many colleagues, advocating for cleaner indoor air in public buildings. Here is a link.
Joe Graedon conducted this interview, as Terry was unavailable.
Listen to the Podcast:
The podcast of this program will be available Monday, Dec. 8, 2025, after broadcast on Dec. 6. You can stream the show from this site and download the podcast for free. This week’s episode contains some additional discussion of outside air, including the dangers of smoke from wildfires, along with particulates from car tires or microplastics.
Download the mp3, or listen to the podcast on Apple Podcasts or Spotify.
Transcript of Show 1454:
A transcript of this show was created using automated speech-to-text software (AI-powered transcription), then carefully reviewed and edited for clarity. While we’ve done our best to ensure both readability and accuracy, please keep in mind that some mistakes may remain. If you have any questions regarding the content of this show, we encourage you to review the original audio recording. This transcript is copyrighted material, all rights reserved. No part of this transcript may be reproduced, distributed, or transmitted in any form without prior written permission.
Joe
00:00-00:01
I’m Joe Graedon.
Terry
00:01-00:05
And I’m Terry Graedon. Welcome to this podcast of The People’s Pharmacy.
Joe
00:06-00:27
You can find previous podcasts and more information on a range of health topics at peoplespharmacy.com. How do you catch the flu, COVID, or cold? Such respiratory infections are transmitted through airborne viruses. This is The People’s Pharmacy with Terry and Joe Graedon.
Terry
00:34-00:46
Dr. Linsey Marr is one of the country’s leading experts on air quality. She was among the first scientists to identify airborne transmission as a problem during the COVID pandemic.
Joe
00:46-00:51
Dr. Marr will tell us how we can improve the quality of the air we breathe.
Terry
00:51-00:58
Do you know how well the air in your home is filtered? What about the air quality at school, at work, or in your doctor’s office?
Joe
00:59-01:07
Coming up on The People’s Pharmacy, how cleaner indoor air reduces your risk of infection.
Terry
01:14-02:16
In the People’s Pharmacy Health Headlines: viruses are on the move, through the air and on surfaces. Subclade K type A H3N2 influenza is spreading. People catch it primarily by inhaling invisible viral particles. Public health authorities are worried that current influenza vaccines may not protect well against this new variant.
The other virus that’s causing a lot of misery is norovirus, also known as stomach flu, the cruise ship virus, or the winter vomiting bug. It’s one of the most easily transmitted infections because just a few particles can make you very sick. Wastewater scan shows a significant uptick in the last couple of weeks. If anyone in your household starts throwing up or having diarrhea, you’re at risk of catching this virus. That’s because it can be transmitted through the air. There is no vaccine or effective treatment against norovirus.
Joe
02:17-03:31
Nutrition experts have been arguing about fat for decades. Starting in the 1980s, Americans were encouraged to follow a low-fat diet. Instead of using butter, people were told to use vegetable oil. Saturated fat was the enemy because it was thought to clog coronary arteries. Hydrogenated vegetable oils were promoted because they had no cholesterol. And seed oils, such as peanut, corn, and safflower oils, became popular because they, too, were low in saturated fat.
In recent years, though, researchers became concerned that hydrogenated vegetable oils contributed to atherosclerosis. And now, researchers at the University of California, Riverside, report on an experiment with soybean oil. Mice fed on soybean oil developed obesity more easily than those fed coconut oil. The investigators identified a liver protein that determines how the body handles linoleic acid, a major component of soybean oil and some other vegetable oils. They point out that many processed foods contain soybean oil, which could be contributing to the obesity epidemic.
Terry
03:32-04:51
Diet can play an important role in controlling blood sugar for people with type 2 diabetes. A study published in the American Journal of Clinical Nutrition demonstrates that slowly digestible starch can be very helpful. Because this slowly digestible starch is metabolized over a long time, it does not lead to spikes in blood glucose or insulin.
Investigators recruited 51 people with type 2 diabetes and randomly assigned them to diets either high or low in slowly digestible starch. For three months, the volunteers kept track of their blood sugar with continuous glucose monitors. They also met with dietitians for nutritional and culinary counseling.
Those whose diets were high in slowly digestible starches such as peas and beans, nuts and seeds, and whole grains had less dramatic changes in blood sugar. Both groups lowered their levels of HbA1c, a medium-term measure of blood sugar. Those on the diets rich in slowly digestible starches actually got their A1c below 7%, which was the target. The researchers believe this offers an effective and accessible strategy to help people with type 2 diabetes gain control.
Joe
04:52-05:44
Australia’s equivalent to the Food and Drug Administration is called the Therapeutic Goods Administration, or TGA. Like the FDA, it monitors drug safety. Recently, the TGA issued a new safety warning to people using GLP-1 drugs such as semaglutide, tirzepatide, liraglutide, and dulaglutide. These drugs have become household names such as Ozempic, Wegovy, Mounjaro, and Zepbound.
The TGA is concerned about reports of suicidal thoughts and behaviors associated with these medications. The regulatory agency is urging doctors to monitor patients for the emergence or worsening of depression, suicidal thoughts, or behaviors, and or any unusual changes in mood or behavior.
Terry
05:45-06:17
Residents of several states are being warned to stay indoors because of poor air quality. High levels of ozone or fine particulates too small to see are making breathing dangerous in many places. You can check your local air quality index at the website airnow.gov. And that’s the health news from the People’s Pharmacy this week. Welcome to the People’s Pharmacy. I’m Terry Graedon.
Joe
06:17-06:27
And I’m Joe Graedon. We’re entering cold and flu season, except there are lots of other pathogens circulating in the air we breathe.
Terry
06:27-06:41
We can’t see them because they’re much too little. Infectious agents such as respiratory syncytial virus, human metapneumovirus, pertussis, and mycoplasma pneumoniae can cause a lot of misery.
Joe
06:42-06:57
And let’s not forget that SARS-CoV-2 has not disappeared. This year, a new variant of influenza A, subclade K, is making people sick, and the flu shot may not protect us as well as we’d hoped.
Terry
06:58-07:26
To find out why air quality matters, especially when pathogens are circulating, Joe talked to Dr. Linsey Marr. She’s a professor of civil and environmental engineering at Virginia Tech, where she leads the Applied Interdisciplinary Research in Air Laboratory. Her research group focuses on the dynamics of biological aerosols like viruses, bacteria, and fungi in indoor and outdoor air.
Joe
07:28-07:32
Welcome to the People’s Pharmacy. It’s so nice to have you back, Dr. Linsey Marr.
Dr. Linsey Marr
07:33-07:37
I am thrilled to be here, to be back on the People’s Pharmacy. Thanks so much for having me again.
Joe
07:37-08:21
Well, you know, unfortunately, Terry can’t be with us today, but I am so pleased to find that you have received so many awards and recognition for the work that you have put in over the last five years, especially with regard to COVID. I mean, you are an environmental engineer, you’ve been involved in bioengineering for a long time. And it seemed like COVID was just waiting for somebody with your expertise to come along. Can you tell our listeners what is an environmental engineer and how did you get interested in aerosol viruses? Cause you were into this field before there was COVID-19.
Dr. Linsey Marr
08:23-09:22
Right. Environmental engineers dedicate their careers to ensuring that we have a clean and healthy environment, whether it’s in the natural environment and also in the built environment. The built environment [is] buildings and roads and other infrastructure.
And so, for example, some environmental engineers focus on clean water. You know, we take it for granted that you can turn on your tap and get clean water that is safe to drink. But that wasn’t always true. And that development was thanks to the work of environmental engineers. Another example is that of clean air.
Air in the U.S. used to be much dirtier in the 1970s. It was heavily polluted by dirty cars and the steel industry and other sources. And environmental engineers are the ones who kind of recognize this and helped lead, I guess, research and actions to help clean it up.
Joe
09:22-09:36
Now, I’m saying that COVID changed your world, but you were already in this field. You were already interested. Tell us how COVID did make a difference in your life.
Dr. Linsey Marr
09:37-10:51
Yeah, I had been studying viruses in the air since about 2008 or 2009. And I got into it mainly, well, for a couple reasons. One, I had been studying traditional particulate pollution in the air. As I mentioned, environmental engineers study air pollution. And then a second reason is that I had a child in the end of 2007, and he had started daycare and was getting sick all the time.
So I really became both fascinated and frustrated by the rapid spread of disease in daycare centers. And so I started reading up on this and found out that we really didn’t know as much as it seemed. And what I did read about how the flu spreads between people, some of it just didn’t really make sense with my understanding of how particles move through the air.
And so my research group started out by going into daycare centers, a health center on campus, and airplanes. We collected air samples, really particles in the air, and analyzed those and found the flu virus present in like half of them. And it was in small enough particles that they would stay in the air for a long period of time, float around, and people could breathe them in. And after several hours, they could breathe in enough to become infected.
Joe
10:51-11:15
So you were already beginning to suspect that viruses could float on the air. And then along comes COVID. And the CDC and the World Health Organization, all these public health experts were saying six feet. As long as you’re, you know, eight feet away from somebody who’s infected, you’re home free, no worries. And you are going, whoa, whoa, wait a minute.
Dr. Linsey Marr
11:16-13:01
Yeah. All of a sudden, all the research I had been doing for the previous 10 years really was here. And I had been studying this because I was worried about a new flu pandemic. It wasn’t flu, but it turned out to be a coronavirus. And then there was this constant messaging about, oh, stay six feet away from people and that’ll protect you.
And I knew from what I had been studying that that was likely not true. And it was based on some older, let’s say, kind of dogma or kind of, yeah, just dogma about how respiratory viruses transmitted, that it was mainly in these large droplets that people cough or sneeze into your face big enough to see. And they’re large enough and heavy enough to fall to the ground within six feet of anyone who coughed them out. So that, if that were true, then if you stayed at least six feet away, then there would be no way that you could come in contact with these, the viruses being emitted by other people.
But it turns out that, you know, based on research I had done earlier and putting together a lot of studies that other people had done, even going back to the 1940s, I knew that people, whether they’re infected with a respiratory virus or not, but that they emit respiratory particles of all sizes, both those large wet ones when you cough, but also smaller stuff when you talk. And even some people when they breathe. And based on older studies, I knew that the virus could be present in those across the whole size range and could also survive in those.
And so the idea of the six-foot distancing, to me, it just didn’t sound like enough. I think it was due to a misunderstanding about how this type of virus would transmit.
Joe
13:02-13:43
What surprises me in retrospect is that the six-foot rule kind of lasted a long time. It made no sense. And I kept wondering, well, where did it even come from? But I think your research and your colleagues’ work demonstrated pretty effectively that these viral particles could float through the air not for a few minutes and not for six feet, but for a long time and a greater distance, a much greater distance. So when did we finally begin to recognize that, Yeah, six feet wasn’t going to be the answer.
Dr. Linsey Marr
13:44-16:17
I think it was a gradual series of kind of research studies and also observations of super spreading and other types of events that helped us realize that six feet wasn’t enough. And I should say that six feet is helpful because it does keep you kind of farther away from the most concentrated plume. If you imagine somebody’s talking, there’s a kind of a plume of air coming out as if they’re smoking a cigarette and you want to stay away from that. So six feet is good for staying away from that, but it’s not going to absolutely protect you from breathing in those smoke or other respiratory particles.
But there were a number of things that happened. So one was that there was that the outbreak in the Skagit Valley Chorale in early March of 2020, I believe, where there was a choir that went through a rehearsal and maybe one or two people were were infected. They didn’t feel quite well. The group, you know, knew that there was this new virus around. And so they avoided shaking hands, touching each other. And yet still something like over 80% of the members of the choir became infected after that practice.
So that to me was one sign of, oh, this thing is probably in the air because it’s really hard to infect that many people just by touching the same doorknob. Even if everybody did touch the same doorknob, you know, after the first few people touch it, you know, any virus that was on there will probably be gone, have been removed.
So that was one thing. And then there was a study that came out of China in a hospital where they did aerosol particle sampling with the types of instruments, the same types of instruments that my group uses, and they found virus in the very small particles. Now, it was the viral RNA, like its genetic signature, it wasn’t infectious virus. And so some people said, oh, well, it’s not infectious. That doesn’t prove anything. But, you know, we know that it’s hard to, it’s really hard to maintain infectious virus when you’re sampling from air. So that was another hint that it could be there.
And then there were, there were additional studies. Finally, I think later that summer, there was a group that sampled air in a hospital where there were patients, and it was more than six feet away from their beds. And they used a newer sampling device that is gentler and help better keep the virus infectious. And they discovered a lot of infectious virus in the air in those samples.
Joe
16:18-16:59
So there was enough evidence that accumulated over those first year or two that people began to recognize. But they didn’t really want to believe it. And in a sense, there was like, well, we don’t want a mask because that’s a pain in the neck. And we aren’t going to change our heating and air conditioning systems. And so nobody really knew what to do about it, including, I think, a lot of the public health people.
We just have about a minute left before we take a break. But have we learned from COVID? Have we made changes that are significant so that it won’t happen again?
Dr. Linsey Marr
16:59-17:33
I think we have learned there’s a totally new discussion about transmission of viruses through the air that used to be completely absent or was reserved for really special cases. But I think now it’s understood to be widely applicable to colds and flus.
And then, for example, I think the CDC, Centers for Disease Control, had a new website where they recommended a certain amount of ventilation, minimum ventilation in rooms. And so that’s progress. That’s something that did not exist before.
Joe
17:34-17:45
Well, when we come back after this break, let’s talk about progress and what we need to do in the future to prevent another pandemic.
Terry
17:45-18:02
You’re listening to Dr. Linsey Marr, Professor of Civil and Environmental Engineering at Virginia Tech. She leads the AIR2 Laboratory, which focuses on the dynamics of biological aerosols, like viruses, bacteria, and fungi, in indoor and outdoor air.
Joe
18:02-18:07
After the break, we’ll learn about other pathogens in the air besides viruses.
Terry
18:07-18:13
Researchers pay attention to the size of the particles that are wafted around indoors. How do they affect our health?
Joe
18:13-18:19
If you have to spend time where there might be a lot of pathogens in the air, are there ways to protect yourself?
Terry
18:19-18:25
Which places are especially dangerous? Are some public places we should be extra cautious?
Joe
18:25-18:29
Air filters might help. How could we improve ventilation and filtration?
Terry
18:39-18:42
You’re listening to The People’s Pharmacy with Joe and Terry Graedon.
Joe
20:40-20:43
Welcome back to The People’s Pharmacy. I’m Joe Graedon.
Terry
20:43-21:01
And I’m Terry Graedon.
Joe
21:01-21:20
Air quality is important for health, but public health experts have not required landlords to install high-efficiency filters or UV lights to eradicate pathogens. Is there anything we can do to monitor air quality and protect ourselves from airborne pathogens?
Terry
21:21-21:47
I was on assignment out of town and could not participate in this interview with Dr. Linsey Marr. She is one of the country’s leading experts on indoor air quality. She’s focused her research on the dynamics of biological aerosols such as viruses, bacteria, and fungi. Dr. Marr is professor of civil and environmental engineering at Virginia Tech and leads the AIR2 Laboratory.
Joe
21:48-22:24
Dr. Linsey Marr, we’ve been talking about COVID, a virus, but there are all kinds of pathogens that float in the air besides viruses like influenza and COVID, SARS-CoV-2. Tell us about the size of the particles, whether it’s a bacteria or whether we’re talking fungi or some other pathogen, and how all of the stuff that’s in our environment, whether it’s inside or outside, may affect our health.
Dr. Linsey Marr
22:26-23:54
Yeah, there’s a whole… world of microscopic organisms in the air around us. And bacteria are around one micron in size. And to put that in perspective, a strand of your hair is probably 50 to 100 microns in diameter. So imagine something that’s one-fiftieth to one-hundredth that size. Fungi might be that size or a little bigger. Viruses are maybe smaller than that bacterium. Maybe like the coronavirus and flu viruses are around 0.1 microns. So one-tenth the size of the bacterium.
But those things do not float around naked. They’re released from a respiratory tract or with bacteria. It might be splashed out of water somewhere, blown out of soil. And so it’s carrying, there’s a particle that is carrying the virus or bacterium or fungi, but often it also, usually it carries other things from that fluid. So like our respiratory fluid, your saliva, sure, it’s liquidy, but if all that water evaporates, you’re left behind with a lot of salts and proteins and other organic material. And in fact, that amount of material, you would have almost like 100,000 times as much of that other material, mucousy, salty stuff, than you would the amount of virus in it.
And so these things are all around us. They’re very tiny. We can’t see them, but they’re there.
Joe
23:55-25:53
Well, you know, you’ve used the metaphor of smoke. And I think it’s really, you know, it’s a great example. If you enter a room where somebody has been smoking a cigar, you will know it instantly because it smells. You probably won’t see the smoke, especially if they were in the room maybe 30 minutes before you walked in and they had left. But the idea that there are still those smoke particles floating through the air and you can smell them, that kind of is a wake-up call that whenever we walk into any room, almost anywhere, there are going to be particles, especially if there are a lot of people in that room.
And I think of concerts. I think of sporting events, basketball season, and thousands of people all screaming their lungs out, some of them sneezing. And I’ve seen your video that you’ve shown with people sneezing, and it’s really scary. And so there are a lot of venues where you’re going to be breathing in a lot of different pathogens.
And the question is, why are some people more likely to get sick than others? We got a lot of email from people who said, oh, I don’t worry about that stuff because my immune system is so good. I take lots of vitamins and nutrients and I can ward off anything. And then I’m thinking, yeah, but what about norovirus? If you walk into a bathroom where somebody threw up or had diarrhea, there are going to be norovirus particles floating through that public restroom. Or what about influenza? Or just, you know, there are so many kinds of pathogens out there. So I guess the question becomes one of, we can’t see this stuff, but it’s there, how do we protect ourselves?
Dr. Linsey Marr
25:54-27:53
We covered a lot in that question. So let me, that’s a great question. Let me go back to the cigar. So what we are smelling is often the gases that are in there, not the actual particles. Although if the gases are present, there may still be a few smoke particles around. And then in terms of kind of particles in the air all around us, there’s even in a room that appears clean, a typical amount of particles in the air, and this is not just like microbial stuff, but just total particles of all kinds, is you would have like a thousand particles per cubic centimeter. And a cubic centimeter is roughly the size of a sugar cube.
So you take a big deep breath in and you’re breathing in like a million particles. And a lot of those come back out, but some of them do deposit. And some of them are salts and other organic material and lots of different materials. Only a small fraction of them are actually microbes. And an even smaller fraction of those are actually pathogens.
And so how do we protect ourselves in these types of places where they’re all around us? Well, the fact that the pathogen is in the air and you breathe it in is only one part of the equation of whether you’re going to get infected and sick or not. Because indeed, your immune system plays a big role here in trying to fight off these pathogens. And that response is going to vary hugely from individual to individual. And that’s outside my area of expertise. But, you know, I work with people who know a lot more about that. And that certainly plays a big role.
And then, you know, how do you protect yourself if you are, let’s say, immunocompromised or you’re on a big, important trip and you don’t want to get sick? Well, you know, for things in the air, you would want to wear a high quality mask, a respirator, something like an N95 that, you know, fits well, especially when you’re in around other people and in crowded, poorly ventilated areas.
Joe
27:55-29:02
And then, let me interrupt… let me interrupt you right there, Dr. Marr, because Americans hate masks. That’s pretty clear. People in other countries, South Korea, for example, China, they’re more than happy to wear masks. But here it’s like, no way. It’s an invasion of my personal freedom.
And, you know, when you get on an airplane, you have to walk through that passageway where I suspect there’s very little in the way of ventilation. And if there are a lot of people getting on the plane, you’re going to be standing in line and you’re breathing everybody’s air. And even on the airplane, it may not be as well filtered as a lot of people would like it to be.
So the culture of masking seems not going to work here in the United States. As soon as people could stop wearing a mask, they did. And people who do wear masks, people sometimes look at them like, “What’s the matter with you?” So how do we change that culture, or is it impossible?
Dr. Linsey Marr
29:03-29:55
Yeah, clearly, you know, American culture is not into wearing masks. That’s for sure. There’s other things we, you know, I don’t know if we how to change that culture, you know, that maybe if we get celebrities wearing them and it becomes cool, that would help get some, you know, advertisers on this to shift the view.
But in the meantime, there are a lot of other things that we can do regarding cleaning the air. As you mentioned, you know, when you’re in the jetway, I’ve, you know, I’ve carried around a little sensor to kind of get a sense for where, where’s the air best ventilated or not. And actually on the jetway, I think because one end is pretty open to the air, you do get decent airflow through there. On the airplane, of course, it’s recirculated, but it’s also very well filtered at the same time.
Joe
29:56-30:19
What are the most dangerous places? Since I assume you’ve been using a CO2, a carbon dioxide monitor, what have you discovered in supermarkets, in doctor’s offices, in pharmacies, wherever you may go and test? Where do we need to be especially cautious?
Dr. Linsey Marr
30:19-31:06
Yeah, I’ve seen the highest numbers in things like restaurants, certain types of restaurants, poorly ventilated ones and crowded ones. Supermarkets, not so much, although I tend to go to the big stores that have really high ceilings and they’re not totally packed with people.
Buses, I would say, I see higher levels. Some classrooms, I’ll see higher levels. So the higher level is an indicator of poor ventilation because carbon dioxide is in our exhaled breath. You do see higher levels on airplanes, but you have to remember that that air is running through filters every two or three minutes. And those filters will remove particles.
Joe
31:07-31:47
Well, speaking of filters, because obviously there are a lot of places where we go where you really can’t test the way you have with your portable CO2 monitor. When you walk into a restaurant, what would you like to see if you had the power to influence public health authorities to actually improve filtration? And then maybe we can talk about how we can start using ultraviolet to kill some of these viruses and bacteria that are floating in the air.
Dr. Linsey Marr
31:48-32:16
I would like to see, and maybe you wouldn’t be able to see it because it would be hidden in the docks and also in the walls, but good filtration systems with the air being circulated a lot of times through that filtration system, and open windows if the weather’s conducive to it so that the air in that restaurant feels as fresh as it does outdoors.
Joe
32:18-32:27
It sounds like Florence Nightingale, you’re sort of adopting her recommendations from more than 100 years ago.
Dr. Linsey Marr
32:28-32:36
She was onto it. She knew what she was talking about. I mean, she observed people getting sick in hospitals and knew how to reduce that.
Joe
32:36-33:05
The only trouble is that most of our public buildings these days are sealed very tight to be energy efficient. And so it’s not always possible to open those windows. Should public health authorities be testing, investigating, making recommendations, and then perhaps requiring public establishments to actually improve filtration and ventilation?
Dr. Linsey Marr
33:06-34:23
Yeah, this is something that a group of scientists and other organizations are working on. I mentioned earlier that the CDC now recommends a minimum ventilation rate of four to six air changes per hour in public spaces. And there was a, I attended an event at the United Nations General Assembly a couple of weeks ago that was intended to raise the profile and spur more action for cleaner indoor air.
And so that, you know, some places will do this voluntarily, but really the way that we get it more broadly installed is through standards and regulations like we do for fire safety. And so we have, you know, a group of scientists has talked about and written a paper that appears in Science about the need for air quality, indoor air quality guidelines and regulations that are widely implemented.
You know, it’s not going to change overnight, but I’m hoping that this starts the discussion and that maybe, you know, 10, 20, 30 years from now, our building stock takes a long time to turn over, but we’ll start designing buildings that are designed not just for energy savings and thermal comfort, but also for good indoor air quality.
Joe
34:23-34:46
Well, at the present time, we can’t always tell. And so what about one of those portable carbon dioxide monitors? Should people be carrying them around with them when they go, for example, into a restaurant or into their local pharmacy? And if the numbers are too high, and what would that be? Maybe turn around and change their mind about going in.
Dr. Linsey Marr
34:48-35:34
Yeah, if you’re someone who’s really concerned about getting sick from respiratory viruses, you could carry one of those around and keep an eye on it for numbers over roughly 1,000 parts per billion. That would be an indicator that the place is not well ventilated. They could, though, have good filtration, which would remove pathogens from the air. So maybe you see that high number, you turn around and go out, or maybe you carry a mask with you and you put on your mask.
So I did hear that I think stores in Japan were required to display their CO2 levels in the window. Something like that would be really helpful for people to be able to see from the outside, oh, what’s it like in there? And then they can decide whether to go in or not.
Joe
35:35-35:56
Oh, that’s a cool idea. I love that idea. You know, having a little electronic sign that says, OK, your CO2 levels here are under 600. It’s like breathing outside air. And then everybody feels, okay, I can go in. And if they’re over 1,000 or 1,500, you say, uh-uh, I’m not coming in today. Don’t thank you.
Dr. Linsey Marr
35:56-36:01
Yeah, I should correct myself also. I think I meant 1,000 parts per million PPM.
Joe
36:01-36:19
That sounds right. Now, one of your colleagues, Dr. Corsi, has come up with a filtration system that’s inexpensive. Not something you can carry around with you, mind you, but something that people could have in their homes or in their offices. Tell us a little bit about that.
Dr. Linsey Marr
36:19-38:01
Yeah, it’s called the Corsi-Rosenthal box, and it acts as a very effective portable air cleaner or filtration unit. Some people call them air purifiers. But it basically mimics what a $200 piece of equipment does for, I don’t know, $60 or so to buy what you need. So one item is a box fan. And then you would also need, let’s see, that’s one, four filters, like kind of those rectangular HVAC filters that you might put into your air conditioning system, you might replace them. And then you tape them together, and you set it on the floor.
So you have this box, this cube, that’s where it’s like the box fan is sitting on top. And it’s pulling air through those filters and then ejecting it out of the top. And what you’re getting out of the top is pretty clean air.
And what’s interesting is that those filters do not have to be HEPA level. So HEPA is high efficiency particulate air filters. Those remove 99.9% or more of particles in the air. They can be slightly less efficient because this thing moves so much air. So even if I have, let’s say I do have a HEPA filter, If I’m barely moving any air through it or trickling a little bit of air through it, it’s not actually cleaning that much air.
But with the Corsi-Rosenthal box, also called the CR box, it’s moving a ton of air through there. So even if it’s only filtering out like 95% of particles, that air is going to go back through the filter and it’ll remove another 95% of the particles. So you get this, you get a benefit of having a high airflow rate through those. And again, it’s inexpensive and you can make it yourself.
Terry
38:01-38:42
You’re listening to Dr. Linsey Marr, Professor of Civil and Environmental Engineering at Virginia Tech. She leads the Applied Interdisciplinary Research in Air, the AIR2 Laboratory. It focuses on the dynamics of biological aerosols like viruses, bacteria, and fungi in indoor and outdoor air.
Dr. Marr teaches courses in environmental engineering and air quality, including topics in the context of global climate change, as well as health and ecosystem effects. She’s been thinking and writing about how to avoid airborne viral transmission since before the pandemic began.
Joe
38:43-38:54
After the break, we’ll find out about the air filters in your home. Do you have a HEPA filter? We’ll also find out about how to interpret MERV numbers.
Terry
38:54-38:59
How well do HEPA filters work? And how often do we need to change them?
Joe
38:59-39:05
Could you kill airborne viruses with UV radiation or ozone? Is that a practical and safe way to go?
Terry
39:05-39:10
Are there any UV systems commercially available for places like hospitals? What about homes?
Joe
39:11-39:18
Dr. Marr will share her list of worrisome airborne pathogens. Flu and measles are obvious. What about norovirus or TB?
Terry
39:28-39:31
You’re listening to The People’s Pharmacy with Joe and Terry Graedon.
Joe
39:40-39:43
Welcome back to The People’s Pharmacy. I’m Joe Graedon.
Terry
39:43-40:01
And I’m Terry Graedon.
Joe
40:01-40:18
Air quality is always important for good health, but because we can’t see pollution or pathogens, we tend to ignore the air we breathe. How would you know about the quality of the air you breathe in your local supermarket, bank, or pharmacy?
Terry
40:18-40:40
Ventilation and filtration are the cornerstones for maintaining air quality indoors. Do you know what kind of filter your air handling system uses? What about at your doctor’s office? When asked why he robbed banks, Willie Sutton said that’s where the money is. When you go to an urgent care clinic or a doctor’s office, that’s where the germs are.
Joe
40:41-40:56
Most people have stopped wearing face masks, and they’re optional at many health facilities. But COVID is still with us, along with influenza, RSV, metapneumovirus, and many other airborne pathogens.
Terry
40:57-41:43
To learn how to improve air quality indoors, Joe spoke with Dr. Linsey Marr. She’s a professor of civil and environmental engineering at Virginia Tech, where she leads the Applied Interdisciplinary Research in Air, AIR2 Laboratory.
Her research group focuses on the dynamics of biological aerosols like viruses, bacteria, and fungi in indoor and outdoor air. Dr. Marr teaches courses in environmental engineering and air quality, including topics in the context of global climate change, as well as health and ecosystem effects. She’s been thinking and writing about how to avoid airborne viral transmission since before the pandemic began.
Joe
41:44-42:25
Dr. Marr, you were talking a little bit about the Corsi… is it Rosenthal box? And how you can do it yourself for a relatively modest amount of money, but you could also put a better filter in your heating and air conditioning system, whether it’s an office building where there are lots of people or whether it’s your home. What are the best filters? You’ve mentioned the HEPA filter, H-E-P-A, but there are also MERV filters. And I’ve never quite got the numbers right. So if you could explain filtration a little more, we’d be grateful.
Dr. Linsey Marr
42:25-44:23
Yeah. MERV stands for Minimum Efficiency Reporting [Value]. I can’t remember exactly what it is. Everyone just calls it MERV. And if you go to a big box store like Home Depot or Lowe’s, they’re going to have filters with their own numbering system on them in terms of how good the filters are. But they should also, you should be able to correlate that with the MERV scale. And the MERV scale is kind of standardized and a higher number is better.
And so it goes all the way up to, I think, 17, which is like HEPA equivalent, um, it starts at one. So I would say, you know, kind of your, and the higher number indicates that it’s going to remove more particles. It has higher filtration efficiency. So the highest ones are going to remove over 99% of particles. And then the lower MERV numbers are really just there to protect your HVAC system from leaves and other big, you know, maybe hairballs from your cat and prevent those from going in.
And so, you know, home systems might have something like a MERV 4 or 8 filter. If you’re getting into commercial buildings, they might have had 8 or 11. But since the pandemic, I think we’ve realized that, oh, having a higher filtration efficiency or better quality filter is, you know, going to give us healthier air for people. And so I think buildings that can are moving more towards MERV 13 or MERV 14 filters.
Now, one caveat here is that the higher efficient, the higher MERV filters that are better removing particles also create a bigger pressure drop. It’s a little harder to push air through those, pull air through those. And so your air handling system needs to be able to handle whatever that filter you put in. So you need to kind of check and make sure your air handling unit is okay.
So for example, we tried this in my house. We tried to put in a higher MERV number filter, but then the system stopped running. It gave me a fault. And so I realized, okay, we’re creating too much pressure drop. We’re asking our fan to do too much work. And so we had to go back down.
Joe
44:25-45:04
So as people begin reinstalling new HVAC systems, whether it’s in an office building, in a supermarket, in a big box store, or at home, they should in the future, hopefully with public health encouragement, design systems that can handle those higher efficiency MERV filters so that we’re up around MERV 13 or above. And how well do they work? Do they really capture enough, let’s say, viruses and bacteria to make a difference? And then how often do they need to be changed?
Dr. Linsey Marr
45:06-46:16
Yeah, once you get up into MERV 13, 14, you’re removing over 80 percent, 90% of particles in the air. And so that’s helpful. But that’s kind of in the mixed air that’s throughout the whole room and throughout the whole building.
Now, we think it’s not clear, but it’s some of the research we’re doing with humans and animals. We think that in a lot of cases, transmission occurs in these closer face-to-face interactions. And in that case, the filter doesn’t help as much because that’s like the whole room air. It’s got to go through the HVAC system and come back before the, and it doesn’t have the chance to do that when you’re talking face-to-face with someone.
So in that case, you need other strategies. But as far as the filters, yes, absolutely. If you’re upgrading your HVAC system, you should be thinking about getting one that can handle the higher efficiency, higher MERV number filters. And then depending on the system. They may recommend filter changes every quarterly, every three months, or maybe semi-annually, so every six months, but it depends on the system. Yeah.
Joe
46:16-46:41
Let’s move beyond filtration and ventilation because that goes along with the filtration. You want to have fresh air being introduced into your system, but let’s talk about killing those bacteria and viruses. What about ultraviolet light? Are there safer systems? What about ozone? Give us an update on how we can purify the air.
Dr. Linsey Marr
46:43-49:11
Right. You had mentioned UV before. And so UV works by killing the viruses or bacteria. It actually messes up their genetic material, DNA or RNA. And so this has been used for decades, a certain type of UV light called germicidal UV, which is at a certain wavelength, 254 nanometers for those who are interested.
The issue with that type of UV light is that it is dangerous for us to look at and it’s bad for our skin to be exposed to it. So those types of systems can only be installed inside air ducts where people are not going to be seeing it and their skin won’t be exposed to it. Or they’ll install it in kind of these upper air systems at the ceiling if they have a high enough ceiling and it’s pointing upward so nobody gets directly exposed to the light.
Now, there’s a newer technology called FAR-UV, and that’s at a different wavelength, 222 nanometers instead of 254. And that is really intriguing because it still kills off viruses and bacteria. And it’s also considered to be eye safe and skin safe. Like it can’t penetrate through the very outer layer of cells in our eyes and skin.
And you mentioned ozone. So UV of any kind can generate ozone also because UV, you’re adding UV light and that generate that kind of can can photolyze or cause chemical reactions with the oxygen and other compounds in the air.
Ozone is bad for us. We have health standards for ozone. And so there’s there’s kind of a trade off here of, well, you have the benefit of killing off pathogens, but you may be generating a small amount of ozone. And, you know, it’s still in the research phases of whether there’s a net benefit and what any long-term effects might be of exposure to far UV.
But it does show a lot of promise. Certainly in laboratory studies, it really effectively kills off pathogens. And, you know, I think of it like we use UV in our drinking water for drinking water treatment in some places instead of chlorination to kill off pathogens. And so this is something, oh, well, we do that in our water. We could do that in our air to kill off pathogens in the air so that we don’t have to breathe them in.
Joe
49:12-49:27
Are there systems now available for, let’s just say, hospitals, for example, or for people’s homes if they wanted to install a UV system? And how would they know if they’re safe? That is to say, not putting out too much ozone.
Dr. Linsey Marr
49:28-50:25
Yeah, I’ve seen there are vendors out there selling far UV lights that you can put in your home. They do recommend that you put them in certain locations in the room. And they have been testing them for ozone. There’s ways you can estimate through there. I know one has a kind of a model where you could put in the dimensions of your room and how many lights you want to put in and what the resulting increase in ozone would be.
So again, we still don’t know what that trade-off is between, okay, you’re removing pathogens from the air, but you’re increasing ozone a little bit. And it’s not just ozone, but the ozone can react and other things that the UV light generates can react with things in the air and produce byproducts that maybe are potentially more harmful and can also produce particles in the air, interestingly.
Joe
50:26-51:10
So it sounds like we don’t yet have a magic wand to be able to purify our air and make everybody safe so they don’t have to think about transmission of pathogens. And while we’re talking about pathogens, if you could just run down the list of things that concern you, because we’ve heard a lot about measles over the last couple of years and how there’s been quite a spread of measles. I do worry about norovirus. I know a lot of people go, oh, that’s just a cruise ship thing, and you can’t possibly get it by breathing. It’s just by touching handrails, for example. But if you could run through some of the pathogens that concern you, please.
Dr. Linsey Marr
51:11-52:59
Certainly. Norovirus is, oh, it’s memorable. I think we don’t know if norovirus transmits through the air. There have been some interesting studies where there was one in Australia in a performing arts locale where the students were going and someone threw up on the carpet. And the next day, a group of students went there and they walked past this spot on the carpet, which had been dried, but I guess not fully cleaned up. And then several students got sick the next day from that stomach bug. So yeah, we don’t know. I wouldn’t be surprised if [norovirus] can transmit through the air. I’m guessing because it’s a gastrointestinal thing, it’s more from touching, but again, we don’t really know.
Other things that are, you know, things that cause the common cold are rhinovirus and adenovirus. Those almost certainly go through the air, although adenovirus can also cause gastrointestinal issues. There’s other coronaviruses. There’s four seasonal types of coronaviruses in addition to SARS-CoV-2, which caused COVID-19. Those can cause colds. We’ve also recently discovered that something called human metapneumovirus is more prevalent than we thought. And that’s just another one of these respiratory viruses that causes colds.
Flu, we should definitely not ignore because that still leads to an average of over 30,000 deaths per year. I think last year was bad. There were 100 or 200 maybe kids who died from it. So we should not forget about flu. Measles, unfortunately, is making a resurgence due to under-vaccination. And that, everyone knows, travels through the air and is very, very contagious.
Joe
53:00-53:21
And I worry about something that seems out of the ancient past, and that’s tuberculosis. I remember talking to an infectious disease expert who said, yeah, TB is not gone. And if somebody is infected, they can spread it pretty fast. Thoughts about tuberculosis?
Dr. Linsey Marr
53:22-54:45
Yeah, I think, you know, I have heard of some cases in the U.S. It’s often in those living in less sanitary conditions and who don’t have regular access to health care because there are treatments, but it requires vigilance, I would say, for the treatments. And so tuberculosis is caused by a bacteria, bacterium that travels through the air.
For sure, we know that this is one of the kind of very well-known, well-accepted airborne diseases because the way it infects is that it has to get down to deep in the lungs because that’s the only place where there’s the right types of cells with the right types of receptors for the tuberculosis, for the bacterium to infect.
Now, another one that we, you haven’t mentioned is Legionella, which I think cases are increasing that’s partly due to greater awareness of it. But this is something that transmits from, not from person to person, but more from water and you inhale it. And so that can be through, you know, it was named after an event in a meeting of the Legionnaires, I think in Philadelphia in the 1970s, but that can be through water that’s contaminated.
There’s outbreaks that have been noted in New York City that are linked to cooling towers on top of buildings where the bacteria grows and then it gets aerosolized in the cooling tower and then can spread throughout the neighborhood.
Joe
54:45-55:02
Dr. Marr, we’re just about out of time. We have about two minutes left. What are you doing for your family and for your students? And what are you recommending to your colleagues when it comes to reducing the likelihood of catching some of these pathogens that we’ve been talking about today?
Dr. Linsey Marr
55:04-55:45
As we mentioned, the carbon dioxide sensor is a good tool. I recently had a colleague who asked me about high levels he was seeing in his office. And we did a little bit of investigation, were able to figure out that air was coming from the hallway and classrooms into his office.
And so, you know, they consulted with the facilities department to try to look into that. They talked about potentially installing an exhaust fan. So, you know, if someone in my family is sick, we will often try to run the exhaust fans, we bring out our portable air cleaner, the HEPA filter unit and kind of it follows that sick person around the house, wherever they happen to be, to try to clean the air and reduce the chances of other people getting sick.
Joe
55:47-56:00
And recommending our listeners should be masking when they’re going into places where there’s the likelihood of people having influenza and colds and other kind of respiratory infections?
Dr. Linsey Marr
56:01-56:27
Certainly during the respiratory season, if you want in the wintertime, if you’re really concerned about getting flus or colds, you’ve got an important event coming up. Masking is going to be probably one of your best defenses, whether that’s traveling on an airplane or you’re in a really crowded area, dense with people. And it seems like the it’s small, the space is small and it’s poorly ventilated, that that will definitely help reduce your risk.
Joe
56:29-57:06
Dr. Marr, we’ve been talking about inside air. Let’s talk about outside air. There’s been a lot of smoke in the air because of forest fires. There has been a lot of other kinds of contaminations. You have looked at a lot of kinds of contaminants in a lot of other places, whether it’s ozone or particulates, even [fluorocarbons or] hydrocarbons. Tell us about outside air and why we should be concerned about it.
Dr. Linsey Marr
57:07-58:13
Outside air is, you know, obviously when we’re outside, we’re breathing that. And a lot of our indoor air actually comes from outdoors. And so, you know, highly polluted outdoor air can come indoors and then we’re breathing it indoors.
So outdoors, there’s things like ozone in the summertime is generated from industrial emissions and also things from motor vehicles and even vegetation contributes to that. We have particles, which are probably the biggest cause of health, have the biggest health impacts in the U.S. and many parts of the world. And those can be generated by combustion and other processes. Interestingly, a lot of them are generated also by reactions involving gases that form particles. And let’s see, you mentioned fluorocarbons. Those are not directly, they don’t directly impact our health, but they can get high into the atmosphere and react with ozone that’s protective, that’s good up there. And so reduce our protective layer of the ozone.
Joe
58:14-58:50
I’ve got one that just struck me a couple of weeks ago: Tires. I mean, you know, there are millions of automobiles and trucks on the road, and we always have to replace our tires after 30, 40, 50,000 miles. And I got to thinking, well, what happens to all of those chemicals and all of that material that is in our automobile tires? Where do they end up? Do they end up in the air? Do they end up in the earth? And how far are they?
Dr. Linsey Marr
58:50-59:34
That’s a great question. In fact, one of my colleagues here at Virginia Tech is looking at that exact question. And he told me a startling statistic about the number of pounds that your tires reduce because of all the tire wear particles when it’s running on the road.
And so a lot of that, if it’s big, chunky, that’s just going to stay on the ground and then it gets washed into our soils or into our bodies of water. Some of it does get into the air. We know that. And so it contains organic compounds and metals and other things. It’s not going to stay in the air forever. Everything in the air eventually has to come back to Earth. But yeah, people are breathing that stuff in, especially, I think, near roadways. But it’s and I think we don’t it’s something we’re still learning more about.
Joe
59:35-01:00:01
And last, microplastic or nanoparticles of plastic or those itsy bitsy little tiny pieces of plastic are everywhere, and they’re in us. Your thoughts about plastic as part of the air, we don’t think of it as something that we breathe because we think, oh, they’re too big, but it seems like plastic is just pervasive.
Dr. Linsey Marr
01:00:02-01:00:37
Yeah, the microplastics are definitely there. They’re going to be worn down into pieces smaller than we can see. They’ve been detected. I had a student who was doing a project in a school and collected dust samples and found lots of microplastics in them.
I think I’m concerned about those, especially because of some of the health studies I’ve seen where you find plastics in the brain and it might be associated with dementia. This is, yeah, it’s an emerging pollutant that I think deserves a lot more attention because it’s something new that we didn’t have nearly as much 50 years ago and really none of 100 years ago.
Joe
01:00:38-01:00:43
Dr. Linsey Marr, thank you so much for talking with us on The People’s Pharmacy today.
Dr. Linsey Marr
01:00:44-01:00:46
Thanks so much for having me. It’s been a real pleasure.
Joe
01:00:47-01:01:27
You’ve been listening to Dr. Linsey Marr, Professor of Civil and Environmental Engineering at Virginia Tech. She leads the Applied Interdisciplinary Research in Air, AIR2 Laboratory, which focuses on the dynamics of biological aerosols like viruses, bacteria, and fungi in indoor and outdoor air.
Dr. Marr teaches courses in environmental engineering and air quality, including topics in the context of global climate change as well as health and ecosystem effects. She’s been thinking and writing about how to avoid airborne viral transmission since the pandemic began.
Terry
01:01:28-01:01:37
Lyn Siegel produced today’s show. Al Wodarski engineered. Dave Graedon edits our interviews. B.J. Leiderman composed our theme music.
Joe
01:01:37-01:01:45
This show is a co-production of North Carolina Public Radio, WUNC, with the People’s Pharmacy.
Terry
01:01:45-01:02:03
Today’s show is number 1,454. You can find it online at peoplespharmacy.com. That’s where you can share your comments about this episode. You can also reach us through email, radio at peoplespharmacy.com.
Joe
01:02:04-01:02:24
Our interviews are available through your favorite podcast provider. You’ll find the podcast on our website on Monday morning. The podcast this week has some extra information about outdoor air, especially when it comes to smoke or forest fires. You’ll also hear about particulates from car tires and microplastics.
Terry
01:02:25-01:02:47
At peoplespharmacy.com, you could sign up for our free online newsletter to get the latest news about important health stories. When you subscribe, you get regular access to information about our weekly podcast. We’d be grateful if you’d consider writing a review of the People’s Pharmacy and putting it on the podcast platform you prefer.
Joe
01:02:47-01:02:50
In Durham, North Carolina, I’m Joe Graedon.
Terry
01:02:50-01:03:26
And I’m Terry Graedon. Thanks for listening. Please join us again next week. Thank you for listening to the People’s Pharmacy Podcast. It’s an honor and a pleasure to bring you our award-winning program week in and week out. But producing and distributing this show as a free podcast takes time and costs money.
Joe
01:03:27-01:03:36
If you like what we do and you’d like to help us continue to produce high-quality, independent healthcare journalism, please consider chipping in.
Terry
01:03:37-01:03:41
All you have to do is go to peoplespharmacy.com/donate.
Joe
01:03:41-01:03:55
Whether it’s just one time or a monthly donation, you can be part of the team that makes this show possible. Thank you for your continued loyalty and support. We couldn’t make our show without you.
Citations
- Morawska L et al, "Mandating indoor air quality for public buildings." Science, March 29, 2024. DOI: 10.1126/science.adl0677

