Exposing Blind Spots
This week, our guest calls attention to beliefs and practices in medicine that are based on dogma rather than data. Why don’t doctors or researchers question these blind spots? You’ll hear about some of the most striking myths, and maybe you’ll be surprised.
You could listen through your local public radio station or get the live stream at 7 am EDT on your computer or smart phone (wunc.org). Here is a link so you can find which stations carry our broadcast. If you can’t listen to the broadcast, you may wish to hear the podcast at your convenience. You can subscribe through your favorite podcast provider, download the mp3 using the link at the bottom of the page, or listen to the stream on this post starting on Sept. 23, 2024.
Exposing Blind Spots:
Our guest, Dr. Marty Makary, defines blind spots as statements that go unquestioned even though they are not supported by evidence. These reveal a medical culture of groupthink. Unfortunately, this is not a new phenomenon. Back in the mid-19th century, Dr. Ignaz Semmelweis investigated the high mortality rate in one maternity clinic he managed. When he found that doctors were going straight from cadaver dissection to delivery, he demanded that doctors wash their hands with disinfectant. His experiment was a great success, since the maternal mortality rate plummeted.
On the other hand, doctors did not believe that washing their hands could possibly make a difference. They refused to adopt the practice, and Dr. Semmelweis became a pariah. Even though this was before people understood the germ theory of disease, the evidence that Dr. Semmelweis had collected was compelling. Despite this, it took more than a century for doctors to accept the necessity of washing their hands before and after every patient.
Surely, an event of this sort could only happen in a benighted era before medicine understood the theory behind infection. At least, so we would hope. However, Dr. Makary cites multiple discoveries that are overlooked for years because they don’t happen to be part of an NIH Center. In some senses, these Centers are silos.
Sticking to Established Standards of Care:
If people are reluctant to stray beyond the accepted wisdom, they won’t make room for new evidence to change how they approach a problem. However, that is the essence of science. Dr. Makary described his participation in grand rounds presenting new information. The committee responsible for overseeing the presentation wanted an assurance that none of the information presented would go beyond the bounds of currently accepted knowledge. He was planning to present new information, which is, after all, the point of education. Consequently, he had to discuss this controversial approach with the committee. It is another way that blind spots get reinforced.
Eggs and Cholesterol:
One medical myth that we have railed against for years is the idea that eating eggs puts your heart at risk. For many years, healthcare professionals maintained that eating foods rich in cholesterol (as eggs are) would raise blood cholesterol. Since elevated cholesterol is a risk factor for heart disease, many people were advised to avoid eggs and to spread margarine instead of butter on their toast. None of those recommendations were based on evidence, but they are among the most persistent blind spots in medicine.
Ulcers and Bacteria:
Another example is medicine’s initial resistance to the idea that stomach ulcers can be caused by bacterial infection, specifically Helicobacter pylori. When Australian gastroenterologist Barry Marshall presented the evidence to his colleagues in 1982, they were slow to stop blaming stress as the primary cause of stomach ulcers. Dr. Marshall persisted and continued to gather evidence. In 2005, the Nobel committee awarded him and his collaborator J. Robin Warren the Nobel Prize for Physiology or Medicine for that research.
Blind Spots on Dementia:
Another ongoing case of doctors doggedly ignoring evidence relates to medications to treat Alzheimer disease. Pharmaceutical firms have spent billions of dollars developing drugs to remove amyloid from the brain, even though the original research that set off the stampede has been questioned. People with Alzheimer disease usually have an accumulation of amyloid plaque in their brains. However, it is not clear whether the amyloid is the principal actor or a bystander of sorts. What is clear is that removing amyloid, as many of these medications do, does not produce impressive clinical benefit. Should medicine rethink this approach?
This Week’s Guest:
Dr. Marty Makary is the chief of Islet Transplant Surgery at Johns Hopkins. A public health researcher, Dr. Makary leads efforts to improve the health of communities and focuses on the “re-design of health care” to make healthcare more reliable, holistic, and coordinated, especially for vulnerable populations. He leads national efforts to increase medical transparency and lower health care costs for everyday businesses and consumers. Dr. Makary is a New York Times bestselling author. He is the recipient of the 2020 Business Book of the Year Award for his book, The Price We Pay. Dr. Makary’s most recent book is Blind Spots: When Medicine Gets It Wrong, and What it Means for Our Health. The website is https://geni.us/blindspots
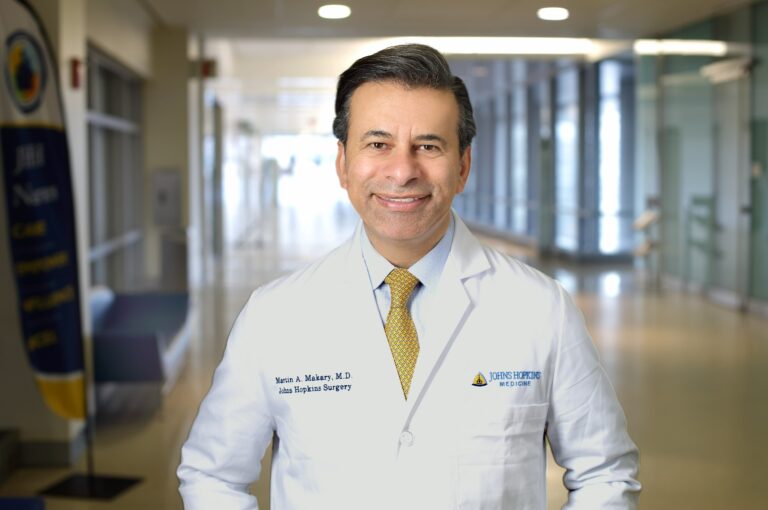
Dr. Marty Makary of Johns Hopkins University
Listen to the Podcast:
The podcast of this program will be available Monday, September 23, 2024, after broadcast on Sept. 21. You can stream the show from this site and download the podcast for free. This week the podcast features additional information on how Johns Hopkins is redesigning healthcare. We also discuss making informed consent truly informed and how treatment guidelines may put patients and providers at odds.
Please Note:
The People’s Pharmacy is reader supported. When you buy through links in this post, we may earn a small affiliate commission (at no cost to you).

