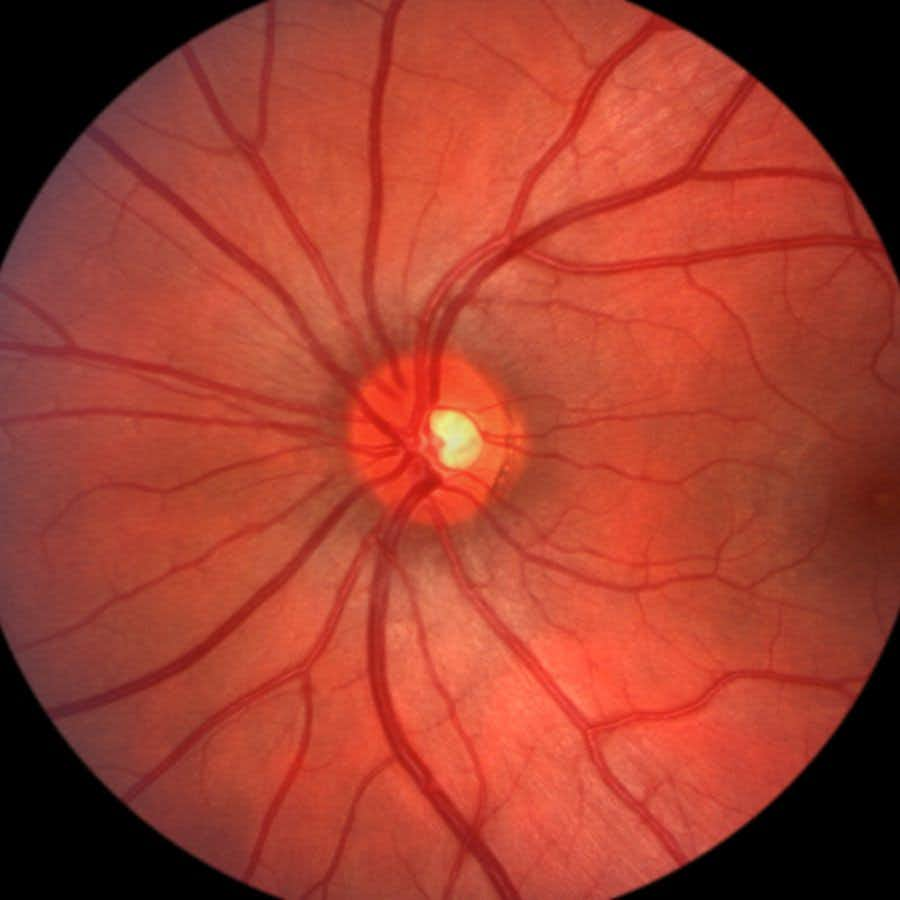
Technology allows for non-invasive imaging of the retina. Now, such a retina scan may allow eye doctors to diagnose Alzheimer disease (see below). If doctors could diagnose neurological dysfunction early, before clinical symptoms appear, they might use a drug like Leqembi to treat patients.
Why Would a Retina Scan Be Helpful?
Previously, scientists found that certain specialized images of the retina could give a sense of what is happening in the brain. The retina gets blood through a dense network of fine blood vessels. In Alzheimer disease, however, this network thins and becomes more sparse. Possibly this reflects what is happening elsewhere in the brain as well.
Earlier research (described below) laid the groundwork. Now, doctors at Duke University Eye Center have demonstrated the feasibility of detecting mild cognitive impairment long before it becomes evident with standard tests (Ophthalmology Science, June 25, 2023).
The researchers used retinal scans called optical coherence tomography (OCT) and machine learning to identify individuals with cognitive impairment. OCT is noninvasive and inexpensive technology that ophthalmologists already use to diagnose glaucoma, diabetic eye disease or age-related macular degeneration.
The senior author states,
“This work brings us one step closer to detecting cognitive impairment earlier before it progresses to Alzheimer’s dementia.”
What Type of Retina Scan Is Useful?
In both this study and the previous one, the scientists utilized both OCT and optical coherence tomography angiography (OCTA). In the earlier study, researchers at the Duke Eye Center compared the retinas of 39 people with Alzheimer disease to the retinas of 37 people with mild cognitive impairment and 133 people with healthy cognitive function (Yoon et al, Ophthalmology Retina, online March 11, 2019).
People with Alzheimer disease had fewer fine blood vessels and one layer of the retina was thinner. These changes did not show up in people with mild cognitive impairment. In the most recent study, however, analysis of retinal images discriminated between people with mild cognitive impairment and those with normal cognition.
Previous Research on Detecting Alzheimer Disease with a Retina Scan:
This is not the first time we’ve heard about the possibility that OCTA may offer early diagnosis for Alzheimer Disease. In addition to the Duke team, scientists at the Goldschleger Eye Institute at Sheba Medical Center in Israel reported markers of the disease that can be seen in a retina scan (AAO 2018, Chicago, IL Oct. 28, 2018). The back of the eye starts to show changes even before people notice serious memory loss.
Ophthalmologists already use OCTA to detect diabetic retinopathy, uveitis, age-related macular degeneration and normal-pressure glaucoma. Impressively, this test is able to distinguish between people with mild cognitive impairment and those who progress to Alzheimer Disease. The Israeli scientists and those at the Duke Eye Center saw the same changes. In conclusion, you could act on an early diagnosis using a retina scan. This would permit earlier intervention to slow or prevent cognitive decline.
Can You Slow Cognitive Decline?
We have heard from many people who say they would not want an early diagnosis of Alzheimer disease because they don’t know of any way to reverse the condition.
Linda sounded a word (or two) of caution:
“I’m all for early diagnosis if the test is conclusive and proven, and there is a treatment protocol. If not, what’s the point of scaring people? We’ve seen the dangers of premature advice on nutrition: the food pyramid that encouraged a high simple carb diet; testing that is so invasive it’s worse than a cure; false positives, etc.
“Now we are in a new health care era in which profit has become the motive, and our medical system is in the hands of insurance companies, some heavily invested in diagnostic testing devices and pharmaceuticals. Look at the profits of colonoscopies, for one thing. They are so profitable that whole buildings are being devoted to them. We have a non-invasive test–Cologuard–available but colonoscopy is still considered the “Gold Standard” even though every part of it has damage potential: the cleanse, the invasive procedure, the anesthetic, and the flexible instrument used.
“A retina scan may prove to be a wonderful diagnostic tool but what happens with the information? And what happens to the patient who is diagnosed with Alzheimer’s that may be years in the future? Or maybe not at all, depending on the conclusiveness of the test after years of being used and, maybe, destroying lots of lives. Who can enjoy life with a diagnosis like that hanging over their head, especially with no clear guidelines to avoid it?
“Technology is a wonderful tool, and it would be so welcome if only we had a health care system in the hands of medical professionals in which good health, rather than profit, was the motive.”
Diane responded:
“Early diagnosis makes sense to me. You could plan for intervention therapy. You could also state the treatment you’d want at a particular stage of Alzheimer’s should it develop.”
Will, a physician, sounded a very hopeful note from New Mexico:
“I see a lot of comments about the lack of treatment for Alzheimer’s. I have been treating patients for the last two years with Dr Dale Bredesen’s methods [see The End of Alzheimer’s]. It’s true that people deep in Alzheimer’s have very little chance of reversal, but we have seen some in early Alzheimer’s and nearly all in Mild Cognitive Decline reverse their condition. MRIs have even documented increases in hippocampal volume. It is real.”
In the meantime, watch out for drugs that could lead to confusion and memory loss. Also, do what you can to avoid insulin resistance, as that appears to increase the risk for Alzheimer disease as well.
Citations
- Wisely CE et al, "A convolutional neural network using multimodal retinal imaging for differentiation of mild cognitive impairment from normal cognition." Ophthalmology Science, June 25, 2023. DOI:https://doi.org/10.1016/j.xops.2023.100355
- Yoon SP et al, "Retinal microvascular and neurodegenerative changes in Alzheimer’s Disease and Mild Cognitive Impairment compared with control participants." Ophthalmology Retina, June 2019. DOI:https://doi.org/10.1016/j.oret.2019.02.002

