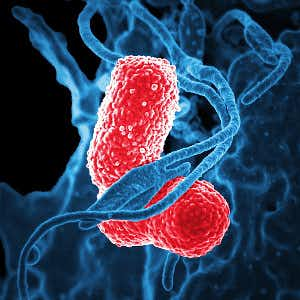
Scientists at the Centers for Disease Control and Prevention (DC) have found bacteria resistant to virtually every known antibiotic in samples from hospitals around the country (MMWR, April 3, 2018). These so-called “nightmare bacteria” were found as part of an effort to analyze samples and detect resistance.
Looking for Carbapenem-Resistant Bacteria:
The CDC hopes to develop strategies to contain the spread of bacteria that are not susceptible to carbapenem and its relatives, considered antibiotics of last resort. That is why it analyzed data from the National Healthcare Safety Network between 2006 and 2015. The analyses showed that the percentage of infections caused by carbapenem-resistant bacteria has dropped during this time, from 10.6% in 2007 to 3.1% in 2015. The agency credits especially strict infection control programs for this decline.
Keeping Bacteria from Spreading Resistance:
Not all the news from this report is encouraging, however. Eleven percent of healthy people who were screened carried superbugs resistant to carbapenem. As a result, these carriers could unwittingly spread their dangerous germs to people with lowered immunity and therefore greater susceptibility to hard-to-treat infections. Such illnesses kill as many as half of those who become infected.
One worry about antibiotic-resistant bacteria is that they can share their scary superpower with other bacteria. In fact, the CDC found that one in four samples had genes that could allow them to spread antibiotic resistance to other microorganisms. That is what makes these bugs nightmare bacteria for public health officials.
Controlling Nightmare Bacteria:
The CDC proposes a containment strategy including stringent infection control measures and rapid identification of antibiotic resistance. It will be up to hospitals to implement much more rigorous infection-control strategies. If properly implemented, such procedures could save lives.

