Many people assume that once they get over COVID they are done! Get on with life and don’t look back seems to be an evolving message that we hear from many visitors to our website. They maintain that we need to learn to live with coronavirus, and stop complaining. The trouble with that concept is that long-lasting COVID complications can upset the applecart. Many people are discovering that long COVID triggers heart problems. The consequences can be devastating. Now scientists are gathering information about exactly how SARS-CoV-2, the virus that causes COVID-19, affects arterial and heart health. The latest news is that a COVID infection can leave some people with an irregular heart rhythm called atrial fibrillation or AFib (AF) for short (Open Heart, Nov. 2023).
COVID-19 and Atrial Fibrillation:
The researchers who published this study in the journal Open Heart compared people who had a diagnosis of COVID-19 between April 2020 and June 2021 to those with non-COVID-19 upper respiratory infections. The authors drew from a very large patient database.
The analysis of patient records from during and before the pandemic shows that people who come down with COVID-19 are more likely to develop atrial fibrillation in the following year than people with other upper respiratory infections. Specifically, 2.2% of those who had COVID were diagnosed with this heart rhythm abnormality compared to 1.2% of those with flu or colds.
That’s a relative risk differential of 83%, which is significant. These results are quite similar to those achieved by comparing people who caught COVID-19 to those who had upper respiratory infections before the pandemic began. People with high blood pressure before a COVID infection were especially susceptible to AFib. In that cohort, 4% of patients were identified with AFib in the year after infection.
Here is how the investigators put their research into context:
“Our results are consistent with prior studies that have examined an association between COVID-19 and AF. In one such study of a large hospital system in the USA, hospitalised patients with COVID-19 were observed to have 19% higher risk of developing AF during their hospitalisation when compared with hospitalised patients without COVID-19. The authors further reported that hospitalised patients with COVID-19 had 57% higher risk of developing AF when compared with hospitalised non-COVID-19 patients during the prepandemic period. In our study, patients with COVID-19 had 83% higher risk of 12-month incident AF as compared with patients with AURI in the pandemic period and 70% higher risk as compared with patients with AURI in the prepandemic period.”
Why Should You Care About Atrial Fibrillation?
It is estimated that as many as 6 million people in the US have AFib. By the end of the decade, that number is expected to rise to over 12 million. Our expert guest on The People’s Pharmacy radio show this coming Saturday (12/2/23) will be discussing atrial fibrillation in depth, so you may want to listen live at 7:00 am EST by streaming the audio signal from one of our radio stations at this link. Or, you can listen to the podcast next Monday (12/4/2023) at this website.
The bottom line is that AFib can lead to stroke and/or death. Symptoms include heart palpitations, fatigue, lightheadedness, shortness of breath or chest pain.
The authors of the latest study linking COVID to AF point out that:
“Growing numbers of AF patients are likely to place additional strain on healthcare delivery systems already impacted by the pandemic and its clinical and financial sequelae.”
The authors are raising the alarm so that healthcare providers will be careful to assess patients for AFib if they have had COVID.
How Long COVID Triggers Heart Problems:
Researchers writing in Nature Cardiovascular Research reveal a new discovery about why people have an increased risk for cardiovascular complications long after an acute infection (Nature Cardiovascular Research, Oct. 2023). They found the SARS-CoV-2 virus directly infecting immune system cells called macrophages in the walls of coronary blood vessels. These foam cells scoop up extra cholesterol when the body is inflamed. Then they contribute to the formation of plaque within the walls of the blood vessels.
Viral infection leads to a persistent inflammatory reaction within arterial plaque formed by foam cells. That, in turn, contributes to heart attacks and strokes. So that is the most recent explanation for how long COVID triggers heart problems.
It is not the first study of this problem, however. More than a year ago, scientists published data on a large number of VA patients who had contracted COVID compared to others who had not.
What About Mild Cases?
Even people who have mild cases of COVID-19 may be vulnerable to long-lasting cardiovascular complications. A study in the journal Nature Medicine (Feb. 7, 2022) tracked data on 153,760 individuals who were diagnosed with a COVID infection at a US Department of Veterans Affairs facility.
These post-COVID patients were compared to 5,637,647 control patients who did not catch COVID. There was an additional control group of 5,859,411 patients from the VA system during 2017 (pre-COVID-19).
Here are the conclusions of the study:
“In this study involving 153,760 people with COVID-19, 5,637,647 contemporary controls and 5,859,411 historical controls—which, altogether, correspond to 12,095,836 person-years of follow-up—we provide evidence that, beyond the first 30 d of infection, people with COVID-19 exhibited increased risks and 12-month burdens of incident cardiovascular diseases, including cerebrovascular disorders, dysrhythmias, inflammatory heart disease, ischemic heart disease, heart failure, thromboembolic disease and other cardiac disorders. The risks were evident regardless of age, race, sex and other cardiovascular risk factors, including obesity, hypertension, diabetes, chronic kidney disease and hyperlipidemia; they were also evident in people without any cardiovascular disease before exposure to COVID-19, providing evidence that these risks might manifest even in people at low risk of cardiovascular disease.”
Translation–Long COVID Triggers Heart Problems That Can Last:
That was a long list of heart problems. They are all serious! These cardiovascular risks persisted for at least a year after recovery.
Let’s explain them:
Dysrhythmias:
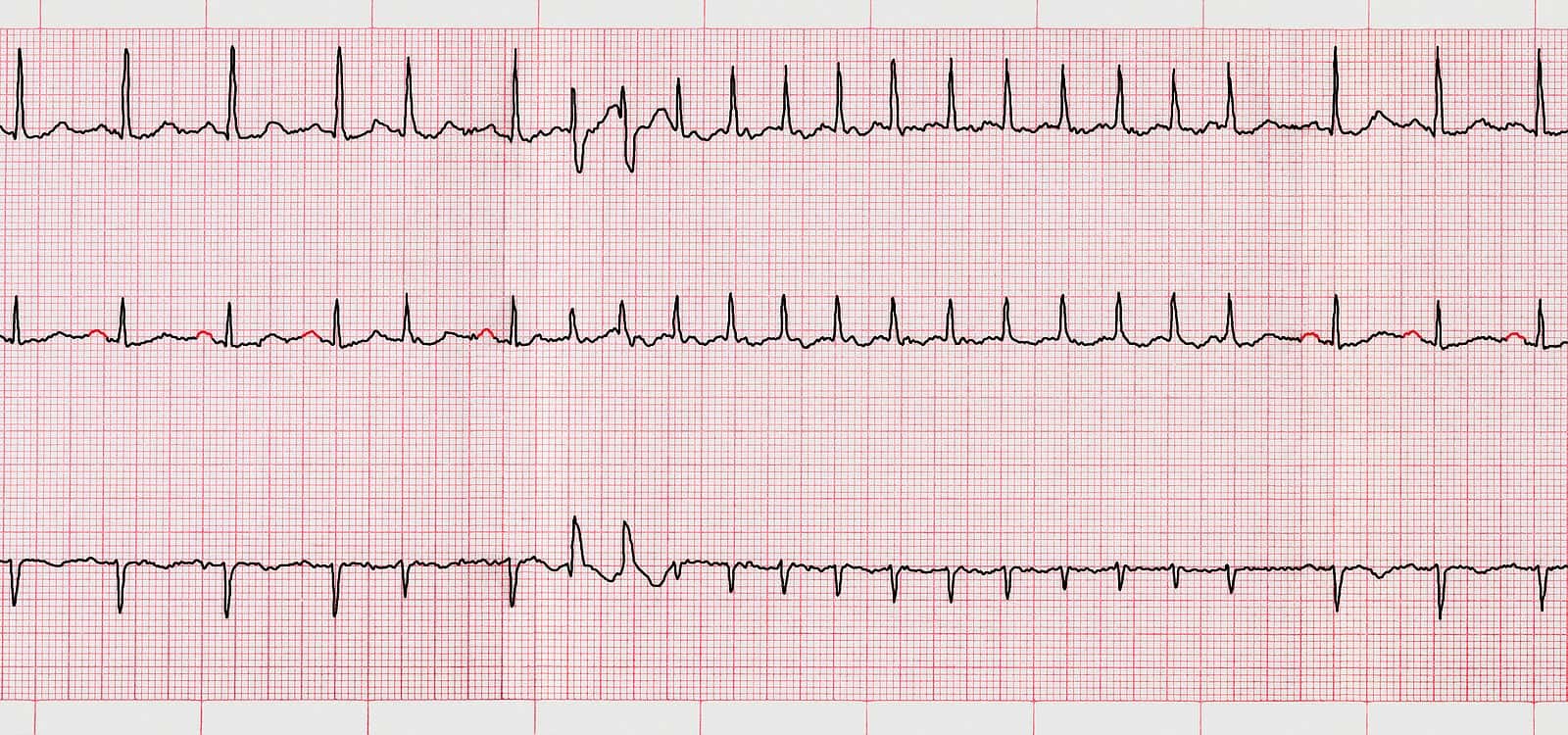
This means problems with either the rate or rhythm of the heart. In the case of COVID, it includes atrial fibrillation, rapid heart rate, slow heart rate and atrial flutter.
Ischemic Heart Disease:
This means reduced blood flow to the heart, angina, heart attack and something called ischemic (reduced blood flow) cardiomyopathy.
Cerebrovascular Disorders:
This means increased risk of stroke, TIAs (transient ischemic attacks or pre-strokes).
Thromboembolic Disorders:
This means blood clotting disorders such as DVTs (deep vein thromboses), pulmonary embolisms (PEs) and superficial vein blood clots.
Other Cardiovascular Disorders:
Heart failure, which means that the heart loses some of its pumping power, non-ischemic (reduced blood flow) cardiomyopathy, cardiac arrest (when the heart stops pumping blood) and cardiogenic shock (when the heart cannot pump enough blood to satisfy the body’s needs).
Inflammatory Diseases of the Heart or Pericardium:
This means that there is inflammation of the heart muscle (myocarditis) or the outer lining of tissue surrounding the heart (pericarditis).
The Bottom Line:
Long COVID Triggers Heart Problems that are serious and can last.
The authors note that:
“Taken together, our results show that 1-year risks and burdens of cardiovascular diseases among those who survive the acute phase of COVID-19 are substantial and span several cardiovascular disorders.”
Final Words:
Please keep in mind that many of the patients with serious heart problems were not hospitalized because of COVID-19. That is to say, they had mild to moderate COVID cases.
We continue to get messages from readers who insist that this coronavirus is just not that big a deal. They do not believe that long COVID triggers heart problems or any other long-term health complications. We are sick and tired of reading that this is all a “scamdemic.”
We wish these COVID deniers would talk to people who are suffering. They could try to minimize long COVID to people who are suffering with the consequences of cardiomyopathy, atrial fibrillation, pulmonary embolism or stroke. We suspect that seeing such distress up close and personal might change some minds.
The authors of this paper point out that:
“…the best way to prevent Long COVID and its myriad complications, including the risk of serious cardiovascular sequelae, is to prevent SARS-CoV-2 infection in the first place. Second, given the large and growing number of people with COVID-19 (more than 72 million people in the United States, more than 16 million people in the United Kingdom and more than 355 million people globally), the risks and 12-month burdens of cardiovascular diseases reported here might translate into a large number of potentially affected people around the world.”
As I write this, more than 419 million people worldwide have caught COVID-19. In the US the number is over 78 million people. That’s according to the Johns Hopkins Resource Center.
The authors of this paper go on to note that health systems around the world need to be prepared for an onslaught of cardiovascular diseases. These serious heart conditions can be long-lasting and will likely require substantial resources.
May we ask for a small favor, please? Google is making it hard for people to search our content. If you found this article of value, please share it with friends or family. You can do that by scrolling to the top of the article and clicking on the icons for email, Facebook or Twitter. While you are at it, please encourage your contacts to subscribe to our *free* newsletter by clicking on this link. Thank you for supporting our work.
Citations
- Eberhardt N et al, "SARS-CoV-2 infection triggers pro-atherogenic inflammatory responses in human coronary vessels." Nature Cardiovascular Research, Oct. 2023. https://doi.org/10.1038/s44161-023-00336-5
- Xie, Y., et al, "Long-term cardiovascular outcomes of COVID-19, Nature Medicine, Feb. 7, 2022, DOI https://doi.org/10.1038/s41591-022-01689-3
- Berman, A., et al, "The association between COVID-19 infection and incident atrial fibrillation: results from a retrospective cohort study using a large US commercial insurance database," Open Heart, Nov. 20, 2023, doi: 10.1136/openhrt-2023-002399

