Irregular heart rhythms (arrhythmias) are cause for concern. Atrial fibrillation (AFib) can lead to fatigue, dizzy spells, shortness of breath and a heart flopping feeling. If uncontrolled, AFib can lead to stroke. Some drugs increase the risk for AFib. Are low vitamin D levels also a risk for atrial fibrillation?
How Would You Know If You Have AFib?
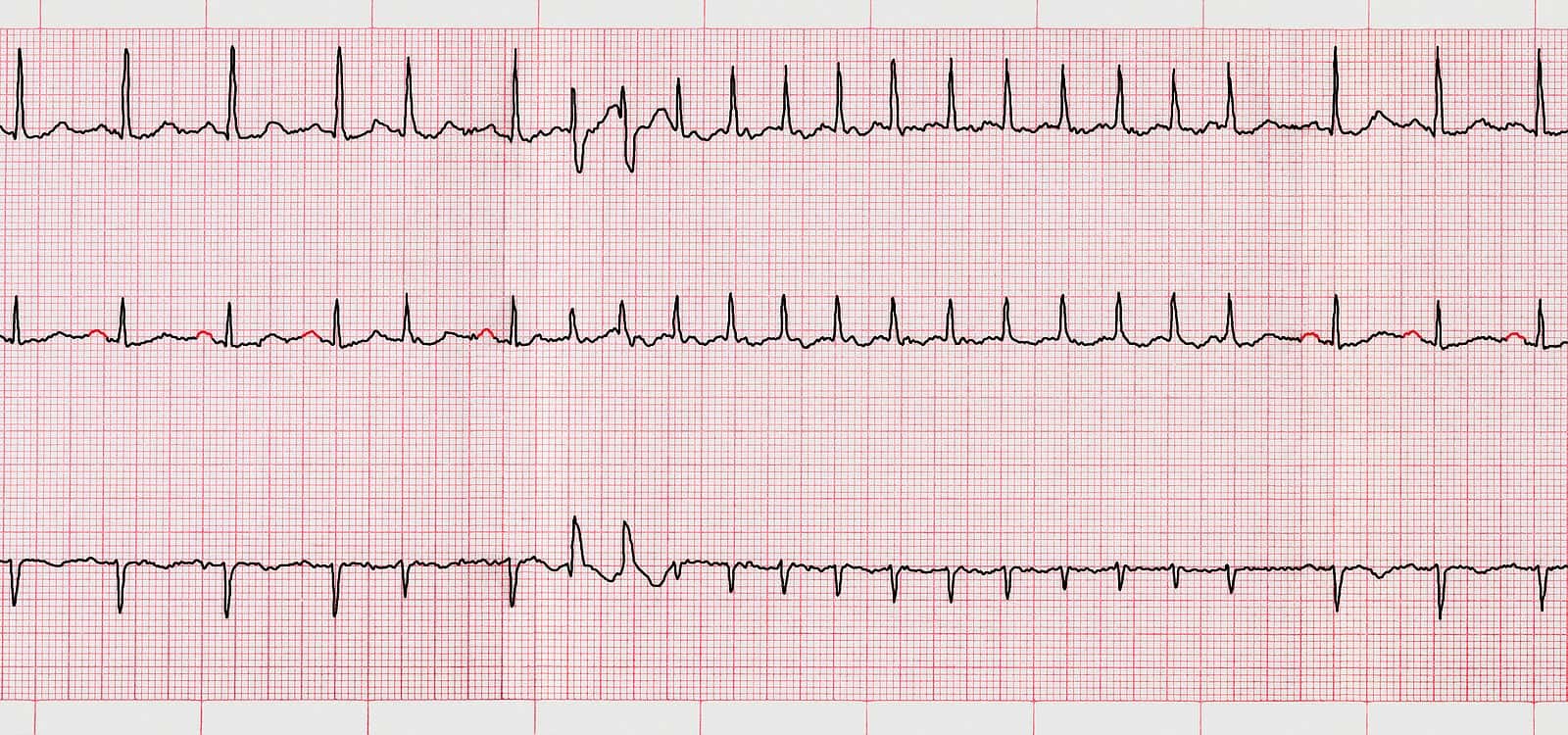
There are now devices such as smart watches or portable heart monitors that can help diagnose this arrhythmia. They’re not perfect, though. An electrocardiogram is a more accurate reflection of heart rhythms.
Anyone with persistent symptoms should be evaluated by a physician. If an Apple Watch detects AFib, a doctor should be consulted.
What Triggers AFib?
A number of medications can increase the risk for atrial fibrillation. Millions of people take corticosteroids (cortisone-type drugs like prednisone) to control inflammation. Tens of millions more take NSAIDs like celecoxib, diclofenac, ibuprofen, meloxicam and naproxen to ease pain. These kinds of medications can put people at greater risk for atrial fibrillation.
PPIs for heartburn may deplete the body of minerals such as magnesium. That too ups the risk for atrial fibrillation. You can read more about pharmaceuticals that could pose problems for this irregular heart rhythm at this link.
Is Your Medicine Triggering Scary Atrial Fibrillation (AFib)?
Atrial fibrillation (AFib) is a potentially life-threatening irregular heart rhythm. A surprising number of medications can trigger this arrhythmia.
Can Natural Approaches Lower Your Risk for Atrial Fibrillation?
Q. I have COPD and an abnormal heart rhythm (AFib). I quit coffee because I read it could trigger AFib. Instead, I start my day with hot water and lemon juice. I also quit drinking alcohol to reduce AFib.
I am trying to increase my exercise bit by bit. Also, I am hoping the lemon water will lower my blood pressure. After two months on lemon water, it’s been around 125/70. I also have incorporated beets into my diet. They are high in nitrate so I am trusting they will also help me control my blood pressure.
Despite COPD, thyroid disease and pulmonary arterial hypertension, I am doing pretty well. I am working with my doctor and hope to rely more on natural foods. Is there any advice you can give me?
A. We applaud your determination to control your abnormal heart rhythm and your blood pressure. Your doctors need to monitor your progress and help you prevent blood clot formation that might cause a stroke.
Coffee Is Confusing:
Researchers admit that the relationship between coffee and atrial fibrillation is confusing. Some studies suggest that coffee consumption increases the risk for arrhythmias while others indicate that it is protective (Nutrients, Aug. 2023).
Could Lemon and Beet Juice Help?
Low-sugar fruit juices such as lemon juice appear to have a beneficial impact on the heart and can improve exercise performance (Nutrition Research Reviews, Sept 1, 2023). A study in the European Respiratory Journal (Dec. 20, 2023) found that nitrate-rich beet juice lowers systolic blood pressure and improves blood vessel flexibility in patients with COPD (chronic obstructive pulmonary disease). It was also shown to improve exercise capability.
Is Vitamin D Deficiency a Risk for Atrial Fibrillation?
Q. I was diagnosed with paroxysmal atrial fibrillation years ago and have taken propafenone SR every day since. If the AFib pops up from time to time despite the propafenone SR, I take a lower-dose regular propafenone tablet. That usually works in about 30 minutes.
In 2020, I needed these rescue tablets more frequently, from an average of two per week to almost five a week in the fall. After the election, it dropped back down. Since then, I’ve been averaging one a week.
I attribute that spike to work stress and political turmoil. The drop might be due in part to less work pressure and the less intense political situation.
One other factor may be playing a role in my reduced AFib episodes. On December 16, my new primary care physician put me on 2,000 IU vitamin D3 daily. Could vitamin D3 play a role in reducing periods of AFib?
A. You’ve suggested an intriguing possibility. Adequate vitamin D levels might indeed reduce the likelihood of atrial fibrillation.
Studies on Vitamin D and AFib:
One analysis of 13 studies concluded that vitamin D deficiency was associated with an increased risk of atrial fibrillation (Nutrition Journal, Nov. 14, 2019). A randomized controlled trial found that high-dose short-term vitamin D supplements helped prevent A-Fib after coronary bypass surgery (General Thoracic and Cardiovascular Surgery, May, 2020).
One of the reasons doctors worry about atrial fibrillation is that patients have an increased possibility of blood clotting when it is not moving properly through all the heart’s chambers. One study recruited 200 people with A-Fib taking anticoagulants to prevent clots (Nutrition, Metabolism, and Cardiovascular Diseases, June 25, 2020). Those with low levels of 25-hydroxyvitamin D were more likely to develop a clot anyway. Such clots are especially dangerous because they can move into the brain and cause strokes.
This research adds weight to the importance of knowing your vitamin D level. To learn more about this crucial nutrient, you may want to read our eGuide to Vitamin D and Optimal Health. This electronic resource may be found in the Health eGuides section of this website.
Share Your Own AFib Story:
Let others know what it’s like to have atrial fibrillation in the comment section below. How have you controlled it?
Citations
- Coppi F et al, "Sex related differences in the complex relationship between coffee, caffeine and atrial fibrillation." Nutrients, Aug. 2023. doi: 10.3390/nu15153299
- Rossi I et al, "Health effects of 100% fruit and vegetable juices: evidence from human subject intervention studies." Nutrition Research Reviews, Sept 1, 2023. DOI: 10.1017/S095442242300015X
- Alasmari AM et al, "Oral nitrate supplementation improves cardiovascular risk markers in COPD: ON-BC a randomised controlled trial." European Respiratory Journal, Dec. 20, 2023. DOI: 10.1183/13993003.02353-2022
- Liu X et al, "The relationship between vitamin D and risk of atrial fibrillation: a dose-response analysis of observational studies." Nutrition Journal, Nov. 14, 2019. DOI: 10.1186/s12937-019-0485-8
- Kara H & Yasim A, "The relationship between vitamin D and risk of atrial fibrillation: a dose-response analysis of observational studies." General Thoracic and Cardiovascular Surgery, May, 2020. DOI: 10.1186/s12937-019-0485-8
- Çakir OM, "Low vitamin D levels predict left atrial thrombus in nonvalvular atrial fibrillation." Nutrition, Metabolism, and Cardiovascular Diseases, June 25, 2020. DOI: 10.1016/j.numecd.2020.03.023

