Reader Alert: I am not an impartial observer of the latest study on stents or bypass surgery. Although my 92-year-old mother (Helen Graedon) did not suffer symptoms of angina, she was talked into angioplasty on December 13, 1996. The cardiologists were impressed that four of her coronary arteries were “clean.” One, however, had a partial blockage.
She was told that angioplasty would be beneficial. She died the morning after her procedure. Several serious medical mistakes led to her horrific death, but had she arrived at this prominent hospital today I would like to believe the cardiologists would not have recommended angioplasty, stents or bypass surgery!
Why the Caution About Stents or Bypass Surgery?
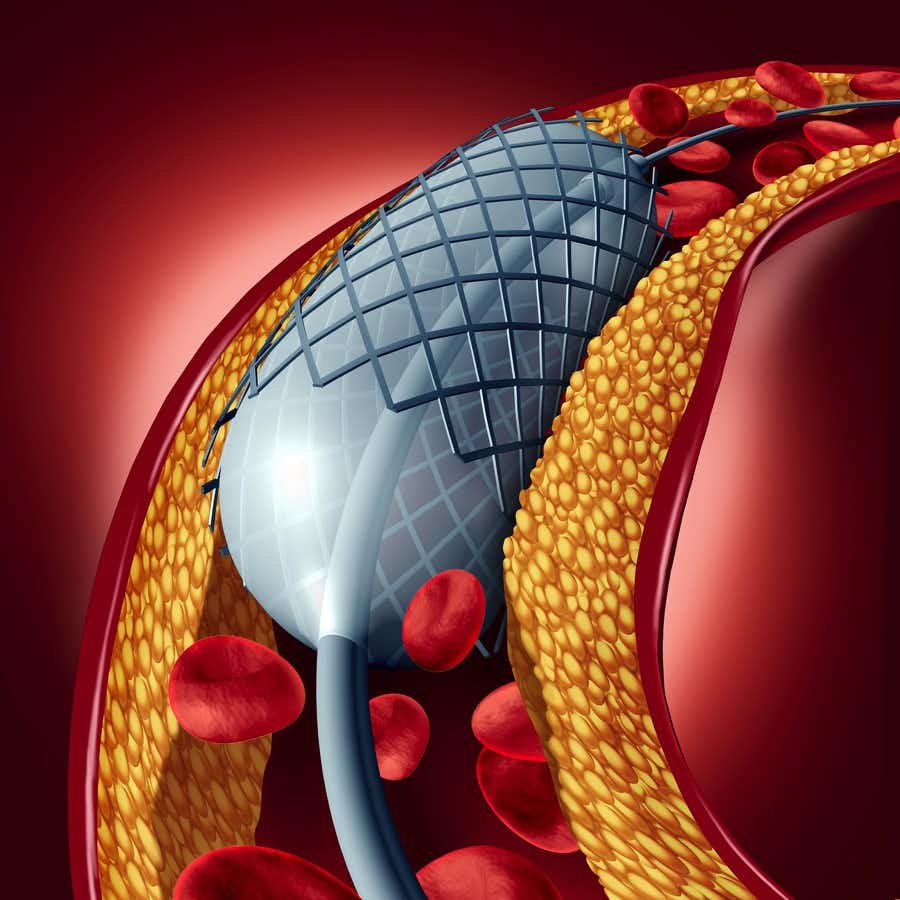
New research challenges the wisdom of routine angioplasty, stent placement or bypass surgery for stable coronary disease. This $100 million study called “ISCHEMIA” involved over 5,000 patients. They all had substantial heart disease.
These high-risk patients were randomized to get either surgery or drugs and lifestyle interventions. After four years, the investigators found that there was no difference in the likelihood of sudden cardiac death, heart attacks or heart failure between the two groups.
Are Cardiologists Salesmen for Stents or Bypass Surgery?
No doubt this important finding will come as a shock to the millions of heart patients who have already had angioplasty, stents or bypass surgery. That’s because such patients have been told for decades that opening a partially blocked coronary artery could save their lives.
A prominent cardiologist we know called this the “oculostenotic reflex.” That’s an insider doctor joke. A commentary in JAMA Internal Medicine (Oct. 2014) titled “Fighting the Oculostenotic Reflex” describes it this way:
“Many physicians are influenced by the so-called oculostenotic reflex, in which any significant stenosis seen during the catheterization is subject to treatment, even if evidence suggests no benefit.”
That’s doctorspeak. What it means in normal language is that if a doctor sees (oculo) some blockage (stenosis) in a coronary artery he is likely to reflexively tell the patient it needs to be treated. And when an interventional cardiologist shows the patient and his family the blockage and adds the overwhelming words: “you’re a heart attack waiting to happen,” most people are easily convinced that they need stents or bypass surgery pronto. That’s even true if they have no symptoms of heart disease.
Why Don’t Cardiologists Believe in COURAGE?
This is not the first time that stenting has fallen short for people with stable heart disease. A study more than a decade ago called COURAGE stunned interventional cardiologists. The researchers randomized 2,287 patients to receive either angioplasty with stent placement or drug therapy and lifestyle changes.
People who got stents to open clogged arteries did not live longer or have fewer heart attacks or strokes than those on medications alone (New England Journal of Medicine, April 12, 2007). This was after five years.
Not surprisingly, many interventional cardiologists objected. After all, this trial challenged a basic premise of cardiology: revascularization by opening clogged coronary arteries was supposed to 1) reduce the risk of a heart attack or stroke and 2) extend life.
Most doctors pride themselves on practicing evidence-based medicine. That means that they do things for which there is solid scientific evidence and avoid things that lack such evidence. One might have imagined that the COURAGE trial would have had a dramatic impact upon the placement of stents or bypass surgery.
Ignoring COURAGE?
Investigators wanted to assess the impact of COURAGE upon interventional cardiology (JAMA, May 11. 2011). They reviewed the medical records of roughly 500,000 patients who had experienced angina because of blockage in their coronary arteries. These people had what is referred to as stable heart disease. That means people experience chest pain or tightness after physical activity or emotional stress. It is “stable” because the discomfort is familiar and is not getting worse.
What the researchers discovered was that only 44% of the patients scheduled for stents or bypass surgery were given what was considered optimal medical therapy (OMT aka drugs and lifestyle interventions). In other words, many interventional cardiologists were ignoring the results of the COURAGE trial and proceeding with a surgical intervention as usual.
In their own words, the authors state:
“Our study demonstrated that less than half of patients undergoing PCI [percutaneous coronary intervention aka angioplasty with stents] are taking OMT before their procedure, despite the guideline-based recommendations to maximize OMT and the clinical logic of doing so before PCI so that the need for additional symptom relief from revascularization can be appreciated. Even after publication of the COURAGE trial, little change in this practice pattern was observed.”
The Scandalous ORBITA Study:
But wait…there’s more! British scientists conducted a study called ORBITA (Objective Randomised Blinded Investigation with Optimal Medical Therapy of Angioplasty in Stable Angina). It was published in The Lancet (Jan. 6, 2018). This study would not have been conducted in the U.S. That’s because most cardiologists would have considered it unethical.
Here’s what the British cardiologists did. They recruited 200 patients suffering from severely clogged coronary arteries. These people experienced chest pain after exercise. All patients were prescribed medications to enhance their heart function. They then were randomized to receive either angioplasty with stents or sham surgery. Yes, you read right. Sham surgery!
How did the Brits perform this sham surgery? The British cardiologists threaded a catheter all the way to the coronary artery and then immediately pulled it out again. There was no angioplasty and no stent inserted in the artery. While it was true that the patients who got angioplasty and stents had better blood flow to the heart, they did not experience less chest pain or better exercise tolerance than the group that got placebo surgery. You can read more details about this extraordinary research at this link:
The Shocking Results of a Heart Stent Experiment
Fast Forward to 2019:
At the American Heart Association Meetings on November 16, 2019, another shoe dropped on the cardiology community. The ISCHEMIA study we described at the top of this post cost $100 million. This was your tax dollars at work.
It demonstrated that stents or bypass surgery do not guarantee protection against heart attacks. Nor do such procedures lead to longer life. Unlike the ORBITA trial, though, there was a difference in quality of life. The group that received revascularization had less chest pain on exertion.
The People’s Pharmacy Perspective:
The ISCHEMIA trial was well done. No doubt some cardiologists will find fault. Keep in mind that interventional cardiologists perform 500,000 stent procedures annually.
Some are absolutely necessary. That is especially true when someone has unstable angina. It can precede a heart attack. Symptoms are worse than usual and include increasing chest tightness, pressure or pain, shortness of breath, sweating, dizziness or nausea. When in doubt, call 911 or go to an emergency department! Further tests will reveal if a heart attack is imminent. In such a situation, stents or bypass surgery may well be called for.
The Death of Helen Graedon:
You can read more details about my mother’s death after angioplasty in our book, Top Screwups Doctors Make and How to Avoid Them. Find out how to prevent diagnostic disasters, prescribing problems, drug interactions and the top screwups in common conditions. Learn how to ask your doctor about the scientific evidence before undergoing procedures.
Helen Graedon was a vibrant, engaged and intellectually curious woman right up until the day she died in one of the best hospitals in the United States. We hope no other family has to experience the horror that we went through during this medical misadventure.
Citations
- Borden, W. B., et al, "Patterns and Intensity of Medical Therapy in Patients Undergoing Percutaneous Coronary Intervention," JAMA, May 11, 2011, doi:10.1001/jama.2011.601
- Brown, D. L. and Redberg, R. F., "Last nail in the coffin for PCI in stable angina?" Lancet, Jan. 6, 2018, DOI:https://doi.org/10.1016/S0140-6736(17)32757-5

