We refer to potassium as the “Goldilocks” mineral. That’s because too much potassium or too little potassium can cause serious health problems. Potassium needs to be “just right.” Normally, the body handles potassium quite easily. As long as you are not taking a medication (such as a diuretic like furosemide or hydrochlorothiazide) that depletes the body of potassium, you should be OK. Ditto for drugs or combinations of medications that raise potassium (such as spironolactone or ACE inhibitors or ARBs). Such drugs can be taken safely as long as potassium is monitored carefully. But many people are not monitored regularly. That can lead to disaster!
Normal or
When is the last time you had your potassium level measured? If you are taking no medicines, that might not be a problem. But if you are taking diuretics and/or certain blood pressure pills, we hope you are getting your electrolytes monitored on a regular basis.
Lowering sodium intake is generally good for cardiovascular health, but increasing potassium intake may be just as important if not more so. A new Danish study (New England Journal of Medicine, Aug. 29, 2025) suggests that people at risk for irregular heart rhythms, especially atrial fibrillation, might benefit from high-potassium foods.
There were 1,200 patients in this trial. They all had either an implanted cardioverter-defibrillator (ICD) or a cardiac-resynchronization therapy defibrillator (CRT-D). In other words, these patients were at risk for serious irregular heart rhythms. They all had an implanted device to shock the heart back into normal rhythm.
The researchers compared usual care to a strategy designed to get potassium levels into the upper end of the normal range. All of these study participants were at high risk of atrial fibrillation and all started with potassium levels at the low end of the normal range.
The outcomes of the study were ventricular tachycardia, a dangerous heart rhythm, or having the ICD kick in appropriately. In addition, the investigators looked at hospitalization for arrhythmias.
The Results of High-Normal Potassium:
The patients assigned to the high-potassium group were prescribed potassium-sparing blood pressure medicines such as ACE (angiotensin-converting-enzyme) inhibitors such as lisinopril. They were encouraged to follow a diet rich in potassium, including foods such as cabbage, beets, white beans, bananas, spinach, nuts and fish. If those steps were unsuccessful at nudging potassium into the high-normal range, the researchers prescribed potassium supplements.
In this vulnerable population, targeting high-normal potassium was helpful. They had significantly fewer episodes of ventricular tachycardia or hospitalization for arrhythmia, and their ICDs activated less frequently. 136 of them experienced such an event, a rate of 7.3 per 100 person-years. In the usual care group, 175 volunteers had one of these dangerous episodes, a rate of 9.6 per 100 person-years. The patients in the high-normal potassium group were also less likely to die during the three years of the study.
The authors concluded:
“In this open-label, randomized trial involving patients at high risk for ventricular arrhythmias who had an ICD, the treatment-induced increase in plasma potassium levels was superior to standard care in reducing the risk of malignant arrhythmias, hospitalization for heart failure or arrhythmia, or death.”
Too Little or Too Much Potassium Can Be Deadly:
Too Little Potassium:
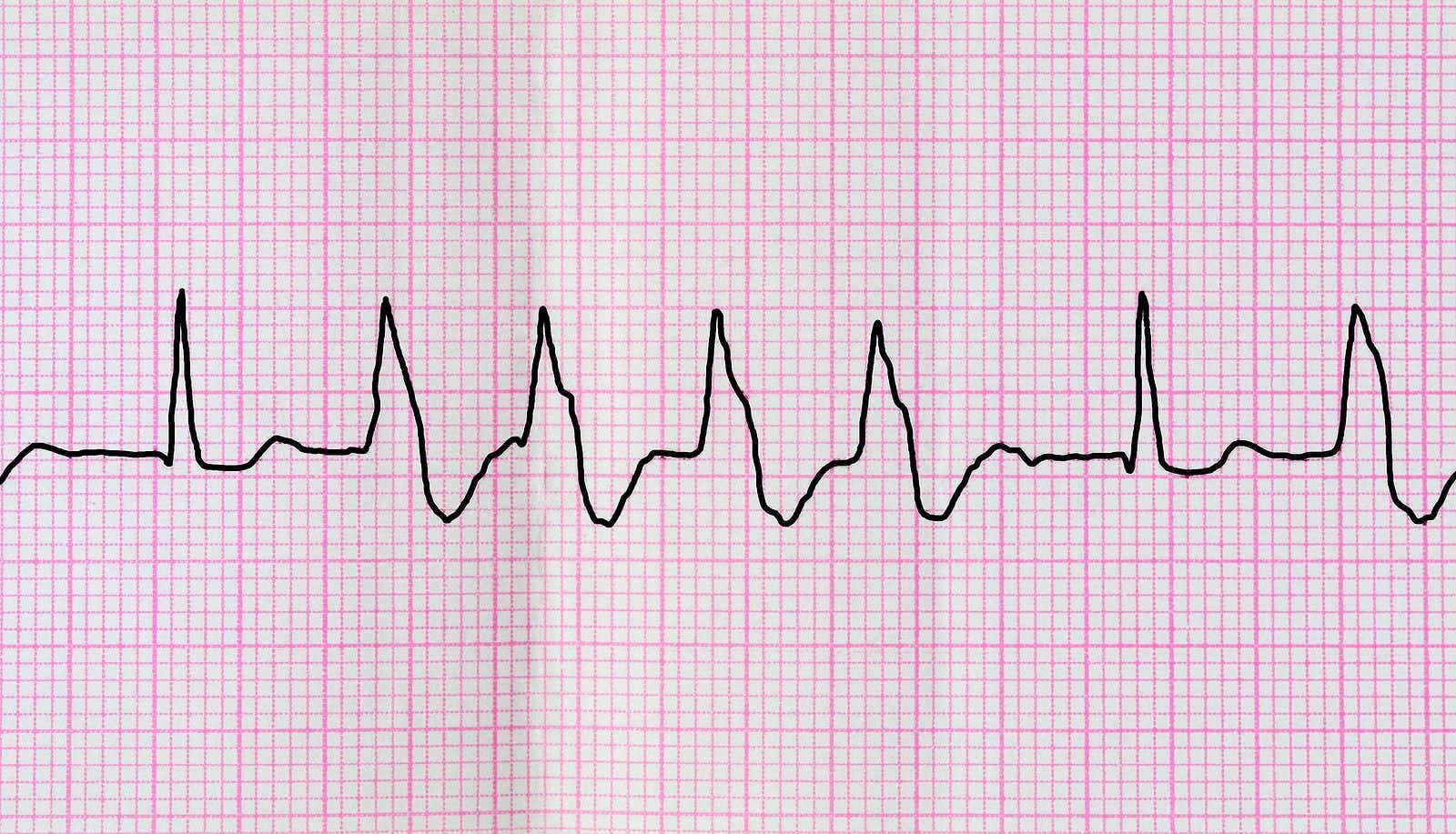
Getting enough potassium is essential for your body to function normally. Too little potassium, HYPOkalemia, can lead to irregular heart rhythms, weakness, muscle cramps, confusion, muscle spasms, numbness, tingling, constipation, thirst and/or frequent urination.
Too Much Potassium:
High potassium levels (HYPERkalemia) can also lead to dangerous outcomes. They may include weakness, slow pulse, heart palpitations, life-threatening heart rhythm disturbances, tingling or numbness in hands, feet or lips and confusion.
If you compare hyper to hypokalemia you will note that irregular heart rhythms can be a feature of both conditions. Ditto for weakness and confusion. The only way to tell for sure is to have blood drawn and get an electrolyte panel.
What Causes High Potassium?
Q. My latest bloodwork shows a potassium level of 5.8, which is considered too high. After trying to find out what I can and cannot eat, I feel I need a registered dietitian.
When I called the practice where I have seen one in the past, the receptionist said their nutritionist wouldn’t deal with that. The same person answering the phone also proceeded to tell me what I could not eat. I found that inappropriate!
Why is my potassium too high? What happens if I ignore it? Are there therapies for this condition? If I can’t get help from a dietitian, who could help me?
A. We agree that it is inappropriate for a receptionist to offer nutritional advice.
What Could Raise This Mineral?
The human body usually tries to keep this crucial mineral within a relatively narrow range, from 3.5 to 5.0 mmol/L. At 5.8, your potassium level is elevated. That is rarely due to eating high potassium foods unless you are also taking a blood pressure medication such as an ACE inhibitor (for example, lisinopril), an ARB (like losartan) or a potassium-sparing diuretic (such as spironolactone).
Other conditions, such as Addison’s disease, kidney disease, diabetes or congestive heart failure can also raise potassium levels. You should ask your doctor to rule these out and to check your medications. An interaction between the BP drug lisinopril and the antibiotic cotrimoxazole (TMP-SMX or Bactrim) can boost potassium levels quickly into the danger zone.
Sadly, this is a drug interaction that may be ignored by many health professionals. You can learn more about this potentially deadly combination at this link.
Emphasizing Symptoms of Too Much Potassium:
I know I sound like a cracked record but potassium goes too high, it can lead to heart rhythm disruptions, chest pain, muscle weakness, nausea, vomiting, diarrhea and stomach pain. In extreme cases, it can lead to cardiac arrest.
You also need a consult with a registered dietitian. Until you see one, make sure you are not using a salt substitute, as it might contain potassium that could readily lead to an excess.
How to Get More Potassium?
Q. I read that potassium is absolutely crucial to reduce hypertension. It suggested 4,700 mg of potassium daily. I don’t think I can eat enough bananas and potatoes to get this much potassium. Is there an over-the-counter supplement I could take?
A. We don’t recommend OTC potassium supplements because you might overdose. This is as dangerous as too little. If you are eating plenty of vegetables and fruits, you are probably getting more potassium than you realize. You can request that your health professional order a blood test to monitor your potassium levels. If that is unsuccessful, you can order your own blood test online and visit a direct-to-consumer laboratory. Here are some examples:
- Labcorp OnDemand Electrolytes Test
- Walk-In-Lab Basic Metabolic Panel
- QuestHealth Comprehensive Metabolic Panel (CMP)
Final Words
Citations
- Jøns, C., et al, "Increasing the Potassium Level in Patients at High Risk for Ventricular Arrhythmias," New England Journal of Medicine, Aug. 29, 2025, DOI: 10.1056/NEJMoa2509542

