How to Treat Common Thyroid Problems
The thyroid gland on your neck is not very big, but it is super important. It secretes hormones that control the activity of every cell in your body. Consequently, the thyroid regulates your metabolism, your heart beats, your bowels and even your thinking. What happens when the thyroid doesn’t work as it should? How do doctors treat the most common thyroid problems?
Autoimmune conditions create common thyroid problems. As a result, levothyroxine (a synthetic thyroid hormone) is the most frequently prescribed medication in the US. In fact, nearly 20 million people have some form of thyroid disease, but not all of them know it. What are the consequences of Hashimoto’s disease and Graves’ disease?
Treating Graves, the Overactive Thyroid:
When the body makes antibodies to the thyroid receptor, the consequence is Graves’ disease. As a result of this attack, the gland makes more thyroid hormone than is needed. As a consequence, a person with Graves’ may have a rapid heart rate, tremors, weight loss, insomnia, heat intolerance, weakness, nervousness and anxiety. Some people with Graves’ disease will develop bulging eyes and eye inflammation. To treat this condition, doctors have medications such as methimazole, radioactive iodine or surgery.
Hashimoto’s and Sluggish Thyroid:
In Hashimoto’s disease, the immune system starts to destroy the thyroid gland and impairs its ability to produce hormones. Consequently, people may feel sluggish and be bothered with constipation. They may have difficulty losing weight and notice that they are losing their hair. Their skin may be extremely dry and they may become extremely sensitive to cold.
Too little thyroid hormone and too much are both common thyroid problems. In addition, doctors generally use a single synthetic hormone to treat hypothyroidism. That’s levothyroxine or T4. However, some people seem to have difficulty converting T4 to the active T3 hormone at an appropriate rate. What can they do?
Have you had experience with a malfunctioning thyroid gland? How was it diagnosed? How did the treatment go? Tell your story in the comments section. You can find our eGuide to Thyroid Hormones here.
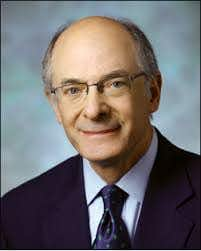
This Week’s Guest:
David S. Cooper, MD, MACP is the Director of the Thyroid Clinic and Professor of Medicine and Radiology in the Division of Endocrinology, Diabetes, and Metabolism at The Johns Hopkins University School of Medicine. His website:
https://www.hopkinsmedicine.org/endocrinology_diabetes_metabolism/index.html
Listen to the Podcast:
The podcast of this program will be available the Monday after the broadcast date. The show can be streamed online from this site and podcasts can be downloaded for free. CDs may be purchased at any time after broadcast for $9.99.

